INTRODUCTION
Schwannomas are typically benign, slow growing, and asymptomatic uncommon neurogenic tumors, and cystic change is extremely rare. In particular, cystic vagal schwannomas originating from the cervical vagus nerve are extremely rare. Standard treatment consists of complete surgical excision of the tumor, with preservation of nerve function through the transcervical approach [1].
Since Gagner [2] introduced the first endoscopic approach, various approaches have been developed and are now used very commonly in Korea. These are especially useful techniques for women who do not wish to be left with a scar on the neck. Recently, we experienced a case of cervical vagal schwannoma with cystic degeneration mimicking a parathyroid cyst that developed in a middle-aged woman. To our knowledge, this is the first case report of endoscopic removal of cervical schwannoma in the English literature. We report a case of cervical schwannoma that was removed via an endoscopic gasless unilateral axillo-breast approach (UABA), along with a review of the relevant literature.
CASE REPORT
A 44-year-old woman was referred to the Otolaryngology-Head and Neck Department due to a slow growing palpable lump at the level of her right thyroid gland. On physical examination, a firm, mobile, non-tender mass measuring 4├Ś4 cm was palpated in the right lower neck without neurological deficit. Ultrasonography revealed a multiseptate cyst measuring 4├Ś3.5 cm (Fig. 1). However, the results of ultrasonography-guided fine needle aspiration biopsy (FNAB) were non-diagnostic, and parathyroid hormone level from the cyst was below the normal range (4.64 pg/mL). Computed tomography (CT) showed a well-defined mass with heterogeneous enhancement and a probable cystic component, and the common carotid artery was splayed apart from the internal jugular vein (Fig. 2).
Blood tests indicated that thyroid function (T3, 92.06 ng/dL; free T4, 1.33 ng/dL; thyroid stimulating hormone, 1.04 ┬ĄIU/mL), calcium (8.1 mg/dL), phosphate (3.8 mg/dL), and parathyroid hormone (43.96 pg/mL) levels were within the respective normal limits. Based on its location and characteristics, our initial impression was that this cystic mass was a parathyroid cyst. The differential diagnoses included a cystic nodule of the exophytic thyroid gland and cervical schwannoma. We planned surgical excision and biopsy for confirmation and to resolve any cosmetic problems. As the patient wanted to receive cosmetic surgery, we removed the tumor endoscopically.
Under general anesthesia, the patient was placed in the supine position. The neck was extended and the arm on the lesion side was raised to fully expose the axillary fossa. A 6 cm skin incision was made parallel to a skin crease in the axillary fossa. The skin was elevated above the pectoralis major muscle under direct vision using monopolar cauterization through the axillary skin incision until the anterior border of the sternocleidomastoid muscle was exposed. To create a working space, an external retractor (Sejong Medical Co., Paju, Korea) was inserted through the skin incision in the axilla and the skin was raised using a lifting device. Another 1-cm skin incision was made along the upper margin of the right mammary areola for the insertion of a 12-mm trocar.
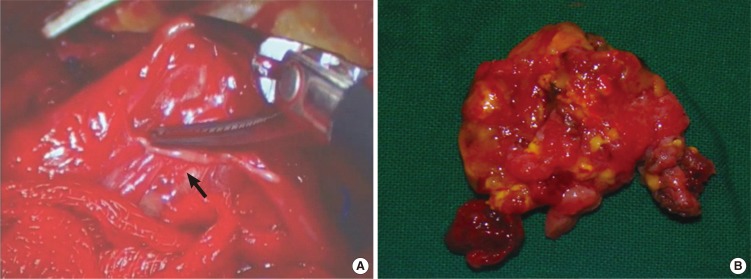
During dissection of the sternal and clavicular head of the sternocleidomastoid muscle, a solid cystic tumor was located between the carotid artery and internal jugular vein. Based on the location of the nerve trunk and tumor, the tumor originated from the right vagus nerve. Under endoscopic view, we carefully dissected the upper and lower ends of the tumor margin and we found the vagal nerve trunk. Using the endoscopic dissector, the tumor was completely removed, with preservation of neural integrity (Fig. 3). Grossly, the tumor was a well-circumscribed, xanthomatous, cystic mass measuring about 3.5├Ś3├Ś0.5 cm. It originated from the right vagus nerve and was dissected using a harmonic scalpel (CS-14C handpiece; Johnson & Johnson Medical, Cincinnati, OH, USA) and an endoscopic dissector. It was separated readily from the surrounding vascular structures.
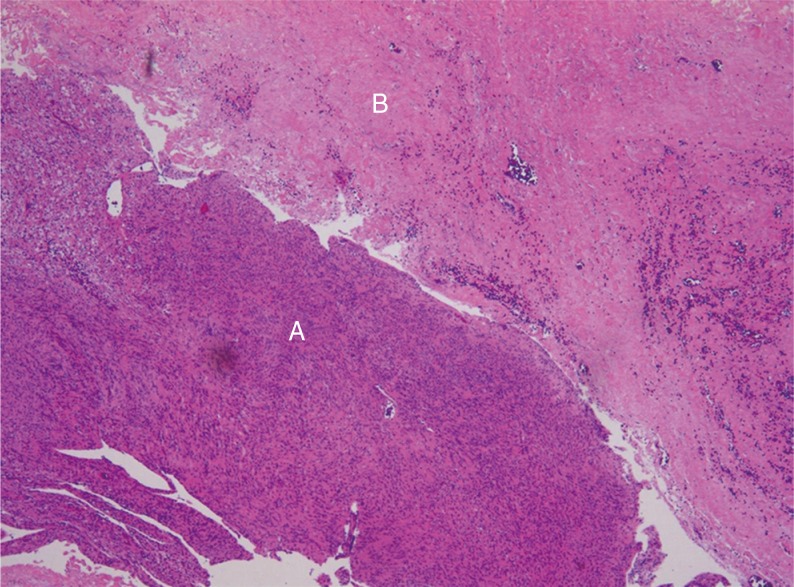
Pathological examination of the tumor confirmed that it was a schwannoma with both a highly cellular component (Antoni A) and a loose myxoid component (Antoni B) (Fig. 4). Although vagus nerve integrity was preserved during dissection, the patient showed temporary vocal fold paralysis on the right side. Postoperatively, we checked vocal cord mobility and found that the right vocal cord was paralyzed. The patient has been followed up for 18 months with no evidence of tumor recurrence or neurological deficit. Vocal cord palsy recovered at 6 months after the operation.
DISCUSSION
Cervical vagal schwannoma is a very rare peripheral nerve tumor, about one third of which occur in the head and neck region [3,4,5]. These are benign, well-circumscribed, encapsulated tumors arising from Schwann cells, a neuroectodermal element of the nerve sheath [6,7]. Cystic changes in vagal schwannoma are extremely rare [1].
Accurate preoperative diagnosis of schwannoma is difficult, because few vagal schwannomas present with neurological deficits, and the differential diagnosis of neck tumors is broad [5]. In this case, we used ultrasonography-guided FNAB, neck contrast CT, and magnetic resonance imaging for preoperative diagnosis. The tumor was initially misunderstood to be a parathyroid cyst.
The treatment for vagal schwannomas is complete surgical excision. Dissection of the tumor from the vagus nerve with preservation of the neural pathway should be the primary aim of surgical treatment of these tumors. Therefore, attention should be paid to preserving the vagus nerve during surgery and a longitudinal incision in the tumor capsule may help to ensure maximum preservation of the nerve fascicles [8]. We used endoscopic gasless UABA for tumor removal. Due to the magnification view, we could dissect the cystic vagal schwannoma from the vagus nerve trunk while preserving neural integrity.
Nerve palsy is a common complication of the vagal schwannoma removal, but in many cases it recovers spontaneously when the neural integrity is preserved. In our case, there was vocal cord palsy, which fully recovered at 6 months after the operation. Endoscopic gasless UABA has many advantages for neck surgery, including no visible scar on the neck and no complications with gas inflation.
In conclusion, we reported an extremely rare case of cystic vagal schwannoma, which was located at an unusual site. We successfully removed the tumor, while preserving neural integrity.