INTRODUCTION
Temporal bone fractures often cause a loss of the audiovestibular function (1). Those patients with bilateral profound sensorineural hearing losses secondary to temporal bone fractures may become candidates for a cochlear implantation (2, 3). Competent assessment of the anatomy and pathology of the middle and inner ears are essential for any patient being considered for a cochlear implant. We present a case of a 65-yr-old male with bilateral profound sensorineural hearing loss caused by bilateral temporal bone fractures who achieved a satisfactory auditory rehabilitation after a cochlear implantation.
CASE REPORT
A 65-yr-old male presented to the emergency department with acute mental changes after a traffic accident on September 16, 2006. He was hit by a car while riding a motorcycle. On physical examination, he exhibited a stuporous mental state. There were positive light reflexes on both sides, but no spontaneous nystagmus. He had bilateral ear bleeding and multiple contusions on his body. An otologic examination revealed a bilateral hemotympanum. The function of the other cranial nerves was impossible to check due to his stuporous mental state.
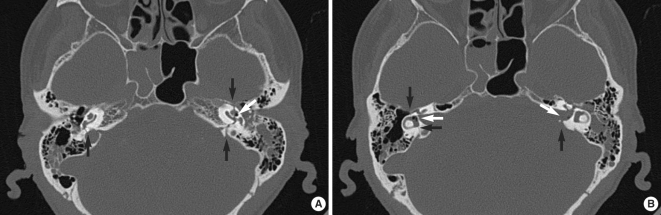
An emergency brain CT scan revealed a hemorrhage in the left temporal subarachnoid space with a pneumocephalus. A high resolution CT scan of the temporal bone revealed bilateral transverse temporal bone fractures involving the otic capsules with evidence of a bilateral pneumolabyrinth (Fig. 1). The fracture line extended to the internal auditory canal on the left side and was associated with a pneumocephalus in the internal auditory canal.
He was admitted to the neurosurgical department for conservative treatment. Two days after the trauma, he exhibited an alert mental state with a complete bilateral hearing loss. No facial asymmetry or weakness was observed.
Audiometry was performed 25 days after the trauma. There was no reliable response to the application of a pure tone or speech stimuli at the maximum limits of the audiometer. Immitance audiometry revealed a type A tympanometry on both sides. Vestibular function testing revealed the absence of any caloric responses bilaterally with ice water.
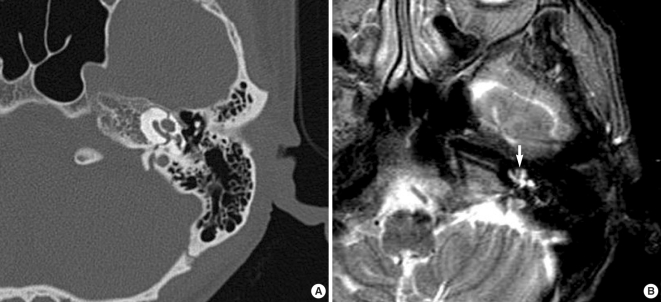
The patient was offered a cochlear implant soon after the trauma. However, he accepted the fact that his deafness was permanent near three months after the trauma and decided to get an operation of cochlear implantation. Follow-up audiometry revealed similar to the previous one, except residual hearing response at 500, 1,000, and 2,000 Hz on the right side. A repeated high-resolution CT scan of the temporal bones was obtained which showed no evidence of labyrinthitis ossificans or obliteration of the mastoid cavity, facial recess, or middle ear space. However, T2-weighted MR image showed a focal low-intensity lesion suggesting fibrosis in the lumen of the left cochlea (Fig. 2). The right ear was selected as the side for the implantation.
He then underwent a right cochlear implant procedure through a transmastoid facial recess approach. A HiRes 90K Cochlear Implant (Advanced Bionics, Boston Scientific) was implanted. The cochlear implant procedure was successful with no evidence of infection and other complications after the cochlear implantation. However, 14 of 16 electrodes were inserted due to the resistance.
Following the mapping, programming, and aural rehabilitation, the patient's listening skills to speech and environmental sounds improved. An implant-aided audiogram three months after the operation revealed responses in the region of 30 dB HL. Still about one and half year after the operation, he always wears the implant and understands 70% of the usual conversation with his family.
DISCUSSION
There are several issues to be considered with cochlear implantations after transverse temporal bone fractures. First, the number of surviving ganglion cells would seem to be a very important factor in determining the success of electrical stimulation (4). Nadol et al. (4) reported an average survival of only a third of the ganglion cell population after temporal bone fractures. Second, the patency of the cochlea after a fracture is another important factor for a successful insertion of electrodes. Transverse fractures may cause direct trauma to the otic capsule resulting in destruction of the organ of Corti and stria vascularis, hemorrhage into the inner ear and subsequent labyrinthitis ossificans (5). Displaced fracture lines and labyrinthitis ossificans associated with temporal bone fractures may complicate the insertion of the electrode array. The most frequent site of an ossification is the basal turn of the cochlea (5). Third, patients with structural abnormalities may have a higher predisposition toward developing meningitis (3). Meningitis is not only a serious disease, but also accelerates the process of labyrinthitis ossificans. Fourth, there is a significant risk of facial nerve stimulation. It is assumed that current leaks from the electrode through the low resistance of the fracture line to stimulate the facial nerve in the region of the geniculate ganglion or in the horizontal portion may occur (2). That may be overcome by programming out the responsible channels.
When there is a significant time delay between the initial CT scan after temporal bone trauma and the cochlear implantation, repeated imaging studies are beneficial to rule out labyrinthitis ossificans or other structural abnormalities such as granulation tissue in the middle ear (6). However, there are no available reports on the prevalence of labyrinthitis ossificans after a temporal bone fracture and the safe time period for no new bone formation. It seems that the sooner a cochlear implant is performed after the time of the temporal bone fracture, the less time is available for labyrinthitis ossificans to occur, and therefore the greater probability for successful electrodes insertion (3). Seidman et al. (7) reported that in up to 22% of cases high resolution CT failed to show a luminal obstruction subsequently found at surgery. T2 weighted MR imaging may be a more sensitive method for determining the patency of the cochlea. Fig. 2 showed similar findings in the present case.
And fracture line on the left side extended to the internal auditory canal. It may have disrupted the eighth cranial nerve, incurring a postganglionic injury and rendering the cochlear implantation useless. Through the careful evaluation of the imaging studies, left side was not recommended for performing the cochlea implantation due to the possibility of direct damage to the eighth cranial nerve and the uncertainty of the patent cochlea.
Cochlear implantations following temporal bone fractures have been proven to have good audiometric and psychoacoustic results, comparable with other etiologies. However, several issues must be considered before performing cochlear implants in patients with profound sensorineural hearing losses caused by bilateral temporal bone fractures. Preoperative imaging studies with both high resolution CT and MRI are highly recommended in patients with temporal bone fractures. This case demonstrated that cochlear implantation with careful planning in such patients can be a very effective method for aural rehabilitation.