|
 |
- Search
AbstractIgG4-related systemic disease, including autoimmune pancreatitis, is a multi-organ disorder characterized by elevated serum immunoglobulin G4 (IgG4) concentration and IgG4-positive plasma cell infiltration. We report a case of a 66-year-old woman with IgG4-related hearing disorder, presenting with fluctuating mixed hearing loss with middle ear effusion. The serum IgG4 level was elevated and pathological examination revealed dense infiltration of IgG4-positive lymphocyte in the renal parenchyma, lung tissue and lacrimal gland. With intravenous methylprednisolone at a dose of 60 mg daily, improvement of hearing loss were observed. No recurrence was observed for 6 months with mainternance of prednisolone and methotrexate.
Immune mediated inner ear disease is occasionally associated with other systemic autoimmune diseases, such as rheumatoid arthritis and Wegener's granulomatosis (1). Immunoglobulin G4 (IgG4)-related systemic disease is proposed to describe systemic manifestation of autoimmune disease characterized by increased serum level of IgG4 and infiltration of IgG4 positive plasma cells in the involved organs, presenting pancreatitis, sclerosing cholangitis, retroperitoneal fibrosis, lymphadenitis, nephritis, interstitial pneumonia, sialadenitis and prostatitis (2-4). We report on a patient who showed fluctuating mixed hearing loss as one of the initial manifestations of IgG4-related systemic disease, which has not been reported before.
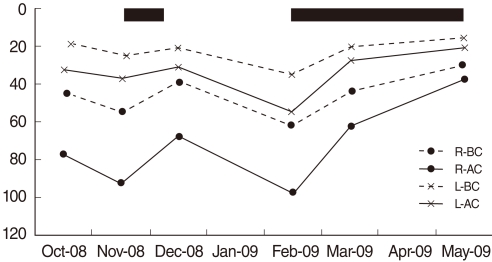
A 66-year-old woman was referred from the neurology department for bilateral tinnitus, hearing loss, and ear fullness that had progressed over the last two months. She also had headache, non-whirling type dizziness, left eyeball pain, arthralgia, and chronic cough. An otoscopic finding showed turbid ear drum in both ears. Four tone average of pure tone thresholds of the right ear were 43 dB (bone conduction) and 77 dB (air conduction), and those of the left ear 17 dB and 32 dB, respectively (Fig. 1, October 2008). Since follow-up audiometry after 2 weeks of treatment of antibiotics showed the disease to have worsened (Fig. 1, November 2008), myringotomy and a ventilation tube was inserted in the right ear. The ear drum and middle ear mucosa was markedly edematous. Spontaneous nystagmus under Frenzel glasses was absent, but an alternating bithermal binaural caloric test showed complete canal paresis of the right side. The direction of nystagmus was not changed with ice water irrigation from supine to prone position. Ophthalmologic examination showed no abnormality. Temporal bone computed tomography (CT) showed partial haziness in the middle ear and mastoid space and thickening of the tympanic membrane and middle ear mucosa. Brain magnetic resonance imaging (MRI) showed abnormal finding in pituitary fossa. It looks like mild pituitary gland enlargement or inflammatory haziness around pituitary fossa. Because of unilateral orbital pain and near the orbital apex lesion on MRI, neurologist suspected Tolosa-Hunt syndrome, and tried steroid therapy (prednisolone 60 mg per day for 25 days and then 30 mg per day for 15 days). During the steroid treatement, her right hearing improved (Fig. 1, December 2008). However, hearing loss was aggravated again (Fig. 1, February 2009) and left eyeball pain and cough relapsed about two months after steroid therapy. A chest CT was checked to evaluate cough, and it revealed multiple nodules in both lower lung fields and renal mass. Orbital CT revealed lacrimal gland enlargement. Biopsies of lacrimal gland, kidney and bronchial mucosa were preformed. Light microscopic examination showed dense lymphoplasma cell infiltration in the lacrimal gland, kidney and bronchial mucosa. Immunostaining for IgG4 showed strong immunoreactivity for IgG4 in infiltrating lymphocytes and plasma cells (Fig. 2). Serologic tests revealed elevated serum IgG of 19.20 g/L (normal range, 3.65 to 9.41 g/L) and elevated serum IgG4 of 2.45 g/L (normal range, 0.061 to 1.1214 g/L). Based on multiple organ involvement, elevated serum level of IgG4, and infiltration of IgG4 positive cells in the pathologic findings, we could diagnose IgG4 related systemic disease. We started immunosuppressive treatments consist of methylprednisolone at 60 mg per day and methotrexate at 12.5 mg per week, and her general condition and hearing markedly improved (Fig. 1, March 2009).
Under maintenance immunosuppressive therapy (prednisolone at 25 mg per day and methotrexate at 15 mg per week), there was further improvement of air-bone gap as well as bone conduction threshold (Fig. 1, May 2009). The dose of prednisolone was gradually tapered and she has been treated with 5 mg daily without further symptoms. We received Seoul National University Hospital Institutional Review Board approval for this study.
The concept of IgG4-related systemic disease has been recognized recently. This disease is known that it involves various organ and can be diagnosed by elevated serum IgG4 level and infiltration of IgG4 positive cells in the involved organs. Since Hamano reported high serum IgG4 concentrations in patients with autoimmune pancreatitis (5), many authors reported multiple organ disease with hypergammaglobulinemia (3, 4). But this is the first report of otologic involvement.
An autoimmune mechanism is assumed in patients with bilateral progressive or fluctuating mixed hearing loss, especially when they respond to immunosuppressive treatment. Similar clinical characteristics were also found in the described patient with IgG4-related systemic disease, which suggests the inner ear can be the target of this systemic autoimmune disease. In addition, the severity of air-bone gap parallels the severity of sensorineural hearing loss, and fluctuates according to the course of immunosuppressive therapy. Therefore, otitis media was a part of this systemic disease and reflecting that respiratory epithelium including middle ear mucosa can be the target in IgG4-related systemic disease. Vestibular dysfunction may progress slowly, hence the patient's dizziness was non-whirling nature without definite history of vertigo or imbalance.
Treatment of this disease is immunosuppressive therapy (2-4). Oral prednisolone is usually started at 30-60 mg/day, and then it is tapered by 5 mg every 1-2 week. Serological and imaging tests are followed periodically after commencement of steroid therapy. Continued maintenance therapy with prednisolone 5 mg/day is sometimes required to prevent relapse without complete discontinuation of steroids (3, 4). In cases of autoimmune inner ear disease, maintenance dose is continued for a variable time but the patients with treatment duration of fewer than 6 months are at increased risk of relapse compared with those treated for 6 months or longer. Immunosuppressant such as methotrexate can be used for recurrent disease (6).
IgG4-related systemic disease is an emerging clinical entity, involving diverse organs and systems including the middle ear and the inner ear. The disease was responsive to immunosuppressive treatment.
References1. Bovo R, Aimoni C, Martini A. Immune-mediated inner ear disease. Acta Otolaryngol. 2006 10;126(10):1012-1021. PMID: 16923703.
2. Kamisawa T, Funata N, Hayashi Y, Eishi Y, Koike M, Tsuruta K, et al. A new clinicopathological entity of IgG4-related autoimmune disease. J Gastroenterol. 2003;38(10):982-984. PMID: 14614606.
3. Saeki T, Saito A, Hiura T, Yamazaki H, Emura I, Ueno M, et al. Lymphoplasmacytic infiltration of multiple organs with immunoreactivity for IgG4: IgG4-related systemic disease. Intern Med. 2006;45(3):163-167. PMID: 16508232.
4. Kamisawa T, Okamoto A. IgG4-related sclerosing disease. World J Gastroenterol. 2008 7 07; 14(25):3948-3955. PMID: 18609677.
5. Hamano H, Kawa S, Horiuchi A, Unno H, Furuya N, Akamatsu T, et al. High serum IgG4 concentrations in patients with sclerosing pancreatitis. N Engl J Med. 2001 3;344(10):732-738. PMID: 11236777.
|
|
||||||||||||||||||||||||||||||||||||||||