Clinical Characteristics of Allergic Rhinitis According to Allergic Rhinitis and Its Impact on Asthma Guidelines
Article information
Abstract
Objectives
The Allergic rhinitis and its impact on asthma (ARIA) guidelines were suggested for use to classify allergic rhinitis (AR). However, few studies have been performed in Asians. The objective of this study is to identify the clinical characteristics of AR in Korean patients according to the ARIA guidelines.
Methods
For the study, 610 patients who had been diagnosed with allergic rhinitis at Seoul National University Bundang Hospital and 545 patients who had been diagnosed with allergic rhinitis at 3 local clinics were included. All the patients were categorized into 4 groups, such as the mild intermittent, mild persistent, moderate-severe intermittent and moderate-severe persistent groups. The patients were given a questionnaire on allergic rhinitis-related symptoms and they underwent blood tests, including the blood eosinophil count and the serum total IgE level.
Results
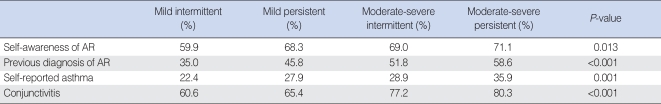
The most prevalent type was the moderate-severe persistent group (34.7%), and the moderate-severe intermittent group (17.1%) was the rarest. There were significant differences among the 4 groups for olfaction (P<0.001), self-awareness of rhinitis (P=0.013), a previous history of AR (P<0.001), self-awareness of asthma (P=0.001) and allergic conjunctivitis (P<0.001). On the allergy laboratory tests, there was a significant difference between the groups for the eosinophi count (P=0.004). The number of blood eosinophil was more in the persistent groups than in the intermittent groups.
Conclusion
According to the ARIA guidelines, the moderate-severe persistent group was the most prevalent for Korean patients. Blood eosinophilia and olfactory dysfunction were the most severe in the moderate-severe persistent group.
INTRODUCTION
Allergic rhinitis (AR) is an upper airway disease that's caused by an IgE-mediated inflammatory reaction after allergen exposure (1), and it could contribute to decreased social activity, a poor quality of school life and decreased productivity in moderate-to-severe symptomatic patients (2-4). Its incidence is 10-25% worldwide and it is on the increase (5) as industrialization progresses. Thus, advanced treatment modalities are required and a more feasible classification system is needed for this propose.
AR had been classified as seasonal, perennial or occupational AR according to the exposed allergens (6). However, the previous classification had some limitations in that it is common that both seasonal and perennial allergens are sensitized and seasonal allergens cause perennial allergic symptoms or even perennial allergens cause allergic symptoms seasonally (7, 8)
The Allergic rhinitis and its impact on asthma (ARIA) group proposed a new classification based on the duration and severity of symptoms. AR is classified into the mild or moderate-severe groups according to the severity of symptoms and AR is also classified into the intermittent or persistent groups according to the duration of symptoms. Thus, AR is divided into four groups: the mild intermittent, mild persistent, moderate-severe intermittent and moderate-severe persistent groups.
In an epidemiological study in a Western country, within the total AR population, 29% of the patients had persistent AR and they had more severe symptoms than the intermittent AR patients (9). In another study in Italy, 1,321 AR patients were enrolled, and mild intermittent AR was diagnosed in 7.7% of the patients, moderate-severe intermittent in 17.1%, mild persistent in 11.6% and moderate-severe persistent in 63.6% (10). Comparison between the ARIA classification and the classical one was performed in France. About 43.7% of the patients who were classified as seasonal did in fact have persistent rhinitis, whereas 44.6% of the patients who were classified as perennial had intermittent rhinitis (11). A retrospective study in 9 Asian countries showed that intermittent rhinitis was observed in less than 20% of patients, whereas patients with persistent rhinitis comprised approximately 80% of the total patients. Although 25-30% of AR patients had mild allergic rhinitis, 60-70% had moderate-severe rhinitis (12).
Most of the previously reported studies included content about the prevalence of the ARIA classification or the difference of the ARIA classification from the classical one. There have been a few studies about the serum total IgE level, peripheral blood eosinophils and olfactory dysfunction in each ARIA group. Twenty one percent of AR patients showed abnormal olfaction in one study, and "blockers" were known to have a significant loss of smell in another study. But there have not been any reports about the distribution of patients with olfactory dysfunction in each of the ARIA groups.
In Korea, the patients with AR are still more commonly managed based on the previous classification rather than on the ARIA classification. In addition, there have been few studies using the ARIA guidelines for Asians. Thus, the objective of this study is to classify the patients using the ARIA guidelines and to compare nasal symptoms, coexisting diseases, olfactory symptoms, the serum total IgE and the blood eosinophil count among the ARIA groups.
MATERIALS AND METHODS
Subjects
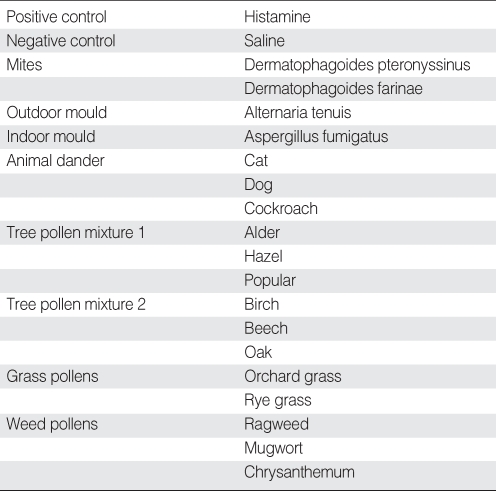
Among the patients with allergic symptoms and who visited the Department of Otorhinolaryngology at Seoul National University Bundang Hospital or 3 local clinics from January 2005 to December 2006, 1,155 patients (610 patients from our institute and 545 patients from 3 local clinics) were included in the study. Patients with deviated nasal septum, chronic rhinosinusitis and nasal polyp were excluded. All the patients were positive for skin prick tests and they were analyzed prospectively by taking their history, conducting physical examinations and administering a questionnaire about AR symptoms. Skin prick tests were performed for 18 inhalant allergens. Saline and histamine were used as negative and positive controls, respectively (Table 1). This study was approved by the Internal Review Board of Seoul National University Hospital.
Diagnosis of AR
The subjects were diagnosed with AR if the wheal size of an allergen was larger than that of histamine on the skin prick tests. According to the kind of sensitized allergens, the patients who were sensitized to tree, grass and weed pollens were diagnosed as seasonal AR, while patients who were sensitized to housedust mites, animal dander and moulds were diagnosed as perennial allergic rhinitis. The patients who were positive to seasonal and perennial allergen were considered as having perennial AR. The skin prick tests were performed with the same method in all the hospitals and clinics.
ARIA classification
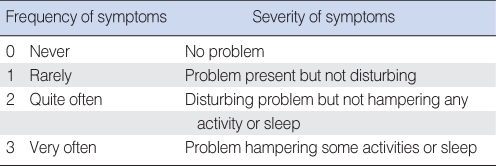
On the basis of the ARIA guidelines, the patients whose duration of allergic symptoms was less than 4 days per week or 4 weeks per year were classified into the intermittent groups and the rest of them were classified as the persistent groups. According to severity, the patients were divided into the mild groups and the moderate-severe groups. A 4-point verbal descriptor scale was used to compare frequency and severity between the groups (Table 2) (9). The patients who mainly complained about sneezing and rhinorrhea were classified into the sneezers and runners, while the patients presented with mainly nasal obstruction, postnasal drip and mucoid discharge were classified into blockers, and the patients with both kinds of symptoms were classified into mixed (13).
Questionnaire for the AR symptoms
The questionnaire was made of 28 questions based on the ARIA classification, and the patients filled this out. The questions included the duration, frequency and severity of the AR-related symptoms, a history of allergic disease, coexisting diseases such as bronchial asthma and conjunctivitis, and the existence of olfactory dysfunction.
Laboratory tests
The serum total IgE level and the percentage of peripheral blood eosinophils were measured in 610 patients. Both the laboratory test results were analyzed for the four AR groups and then these were compared between each group.
Statistical analysis
Comparisons between the previous classification and the ARIA classification were analyzed by chi-square tests and the AR symptoms and laboratory tests were compared among groups through the ANOVA method. Statistical analysis was performed with SPSS (version 12.0, SPSS Inc, Chicago, IL, USA) and statistical significance was set when P values were less than 0.05.
RESULTS
ARIA classification
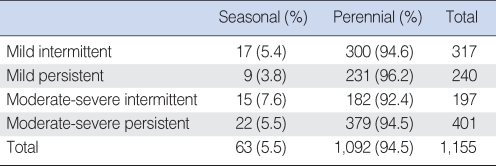
The total of 1,155 patients consisted of 675 men and 480 women. Their mean age was 18.4 and 22.8, respectively. The moderate-severe persistent group accounted for 34.7%, the mild intermittent group 27.4%, the mild persistent group 20.8% and the moderate-severe intermittent group 17.1%. The previous classification according to the time of exposure was compared with the ARIA classification (Table 3). Perennial AR comprised more than 90% of all the AR patients in all the four types of ARIA classification. There was no significant difference among the ARIA groups for the proportion of perennial and seasonal AR (P>0.05). Almost one third of the AR patients had both sneezer and blocker symptoms in all the 4 groups. The number of sneezers (31.2%) was similar to that of the blockers (29.7%) in the mild intermittent group, while the sneezers (36.5%) were more numerous than blockers (27.9%) in the moderate-severe intermittent group. On the other hand, blockers were more numerous than sneezers in the two persistent groups (P=0.012) (Table 4).
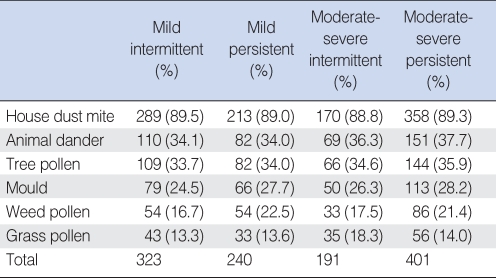
Sensitized allergens
The most common allergen was housedust mites, followed by animal dander, tree pollens, moulds, weed pollens and grass pollens in the 4 ARIA groups (Table 5).
Serum total IgE and blood eosinophils
The average blood eosinophil count was 5.81% in the moderate-severe group and it was highest among the 4 ARIA groups. The blood eosinophil count was higher in the persistent groups than that in the intermittent groups (P=0.037). It was 4.87% in the mild intermittent group, 4.80% in the moderate-severe intermittent group, 5.46% in the mild persistent group and 5.81% in the moderate-severe persistent group. However, the serum total IgE level was not significantly different among the groups (P=0.945). It was 411 in the mild intermittent group, 391 in the mild persistent group, 429 in the moderate-severe intermittent group and 405 in the moderate-severe persistent group (Fig. 1).
History of allergic disease
Self awareness of AR, a previous diagnosis of AR, self awareness of bronchial asthma, a previous diagnosis of bronchial asthma and allergic conjunctivitis were compared among the 4 ARIA groups (Table 6). Self awareness of AR and a previous diagnosis of AR were lowest in the mild intermittent groups. Self reported bronchial asthma was most prevalent in the moderate-severe persistent group (35.9%). Coexistence of allergic conjunctivitis was found more frequently in the moderate-severe groups than in the mild groups (P<0.05).
Olfactory dysfunction
Hyposmia or anosmia was found most commonly in the moderate-severe persistent group (Fig. 2). Olfactory dysfunction was found in 39.3% of the patients in the mild intermittent group, in 45.4% of the patients in the the mild persistent group, in 47.6% of the patients in the the moderate-severe intermittent group and in 61.4% of the patients in the moderate-severe persistent group. There was a significantly higher frequency of olfactory dysfunction in the blockers than that in the sneezers and runners (P=0.001). There was no significant difference of the peripheral eosinophil count and asthma for olfactory dysfunction among the 4 ARIA groups (P=0.311, P=0.132).
DISCUSSION
The most common group according to the ARIA classification was moderate-severe persistent in this study, which is similar to the previous studies that reported on Westerners (14). In the European study for ARIA classification, the most common group was the moderate-severe persistent group (51.2%), followed by the moderate-severe intermittent group (41.8%), the mild intermittent group (3.9%) and the mild persistent group (3.1%) (15). There was no statistically significant relationship between the previous seasonal/perennial classification according to the time of exposure and the ARIA classification.
House dust mites were predominantly the most common allergen in all the groups. House dust mites accounted for almost 90% of the sensitized allergens. The data shows many patients were sensitized to multiple allergens because the sum of the proportion of allergens reached nearly 200% in each group. In other words, the seasonal or perennial AR patients were simultaneously sensitized to seasonal and perennial allergens. For this reason, the previous classification according to the time of exposure does not properly represent each group of AR patients (9, 16). Therefore, it is reasonable to group AR patients according to the symptom duration and severity based on the ARIA guideline.
Although the ARIA classification have been applied and investigated all over the world, there have been few studies on the laboratory differences among the 4 ARIA groups. Our study shows that there was a statistically significant difference between the groups for the peripheral blood eosinophil count (P=0.004). Blood eosinophils were more abundant in the 2 persistent groups than in the 2 intermittent groups. Interestingly, the eosinophil count did not show any difference between the mild and moderate-severe AR groups. In other words, the eosinophil count may reflect the symptom duration of AR rather than the symptom severity. On the contrary, although the serum total IgE was increased, it was not significantly different among the groups.
With regard to the AR-related symptoms, the difference of olfactory dysfunction among the 4 ARIA groups has not been reported on, although olfactory disorder caused by AR is one of the main concerns for otorhinolaryngologists. Olfactory loss can be caused by both conductive and sensorineural mechanisms. Long standing allergic inflammation as well as immediate allergic reaction can induce mucosal hypertrophy and swelling, resulting in blocking of the passage for odorants to be delivered from the atmosphere into the olfactory neuroepithelium. Olfactory receptor neurons can be irreversibly damaged by inflammatory mediators or oxidative free radicals, which may be released by allergic inflammatory cells. Reduction of the olfactory receptor neurons and displacement of the olfactory neuroepithelium by respiratory epithelium culminate in sensorineural loss of olfaction. Olfactory dysfunction was the most common in the moderate-severe persistent group and it was least common in the mild intermittent group. This finding may reflect that AR-induced olfactory loss is related with both the symptom duration and severity. The sensorineural loss of olfaction might be more related with the moderate-severe persistent group than with any other group, which could explain the more frequent loss of smell in that group.
CONCLUSIONS
This study is the largest study to analyze the ARIA classification of Korean AR patients. The study showed the moderate-severe persistent group is the most prevalent, the same as for Westerners. House dust mites were more prevalently sensitized allergens in Koreans than in Westerners. The laboratory tests demonstrated that the blood eosinophil count may be related with AR symptom duration, while the serum total IgE does not play a different role in 4 ARIA groups. The highest prevalence of olfactory disturbance in the moderate-severe persistent group was one of the most characteristic findings of this study. The ARIA classification might be more related with AR symptoms, the prevalence of asthma, olfactory loss and the laboratory tests results than the previous classification, and so the ARIA classification should be clinically applied to all the patients. Further, it should be investigated for determining the proper therapeutic approaches depending on this classification system.
Notes
All the authors have no conflicts of interest for this study.