INTRODUCTION
Sclerosing polycystic adenosis (SPA) is a rare salivary gland lesion that was first described by Smith et al. [1]. Most cases of SPA have originated in the parotid and submandibular glands, with a few cases of minor salivary gland origin [2,3]. We present a case of right nasal cavity SPA in a 49-year-old man with nasal obstruction. This is the first case in the English literature of SPA involving the nasal septum.
Although SPA has a favorable outcome, the histologic findings of SPA include atypia ranging from mild dysplasia to carcinoma in situ, which leads to difficulties in diagnosis and subsequent management. Thus, SPA could be included as a possible etiology of a mass in the nasal septum.
CASE REPORT
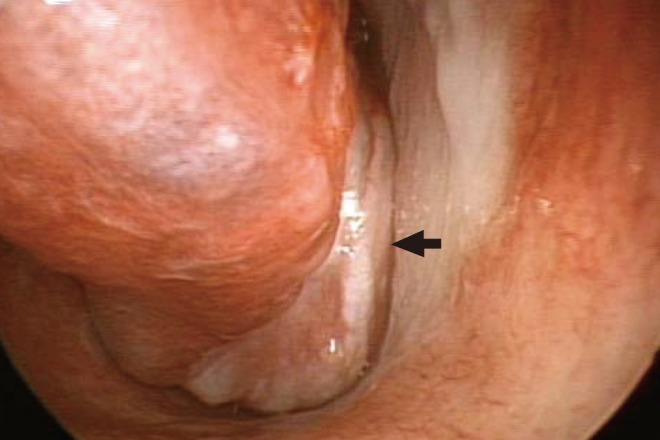
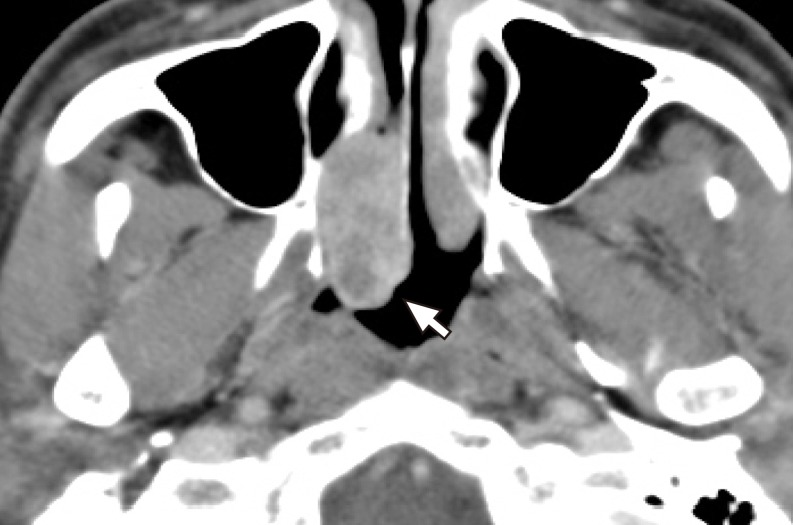
A 49-year-old man presented with a 1-year history of right nasal obstruction and occasional epistaxis. His general health was satisfactory and there was no history of nasal surgery. Nasal endoscopy revealed a 1.5×2 cm mass in the right nasal cavity. The mass was pedunculated, red, and had an irregular surface. The mass arose from the right nasal septum and bled easily on touch (Fig. 1). A computed tomographic scan of the paranasal sinuses showed a polypoidal mass with attachment to the bony nasal septum without erosion into the surrounding structures (Fig. 2). The differential diagnosis included a hemangioma and a minor salivary tumor. A preoperative punch biopsy of the mass suggested the diagnosis of SPA. The lesion was completely excised under endoscopic endonasal surgery under general anesthesia. A margin of normal mucosa and the underlying perichondrium was widely excised.
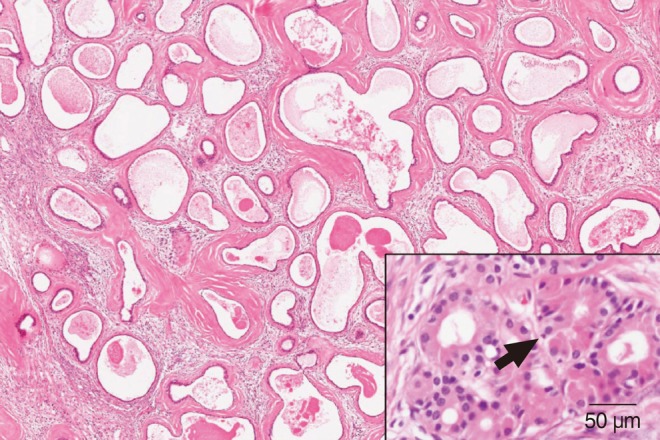
Grossly, the tumor was a firm pedunculated mass, measuring 2.1×1.5×1.1 cm, with a peduncle 4 mm in length. The cut surface was lobular and glistening, containing a few tiny visible cysts <1 mm in diameter. The microscopic examination revealed a subtle lobular proliferation of dilated ductal components with cystic changes surrounded by abundant dense hyalinized hypocellular collagen stroma with a mild inflammatory cell infiltration. The ductal epithelial cells were flattened and cuboidal without atypical features. Frequent apocrine metaplasia was noted (Fig. 3). Immunohistochemical staining for α-smooth muscle actin demonstrated myoepithelial cells surrounding ductal epithelium and the epithelial cells lining ducts showed focal immunoreactivity for estrogen receptor (Fig. 4). Together, these findings were characteristic histopathologic features of SPA. The patient was discharged the next day, and the postoperative course was uneventful.
Postoperatively, no wound complications were observed and no recurrence was observed at the 12-month follow-up examination.
DISCUSSION
Smith et al. [1] described nine cases of histologically-distinct lesions of the salivary gland and suggested the term SPA for these rare lesions. They described the histologic features as a generally lobular proliferation of ductal and acinous elements, cystic ducts with frequent apocrine- and sebaceous-like cells, eosinophilic intracytoplasmic granules within some acinar-type cells, intraductal epithelial hyperplasia with occasional collagenous spherulosis, and dense fibrosis that is frequently nodular.
Approximately 41 cases of SPA have been reported in the literature. Thirty-four tumors arose in the parotid gland, three envloved the submandibular gland, and four arose in the oral cavity mucosa [2-5]. This is the first reported case of SPA of nasal minor salivary gland origin. Based upon previous reports, SPA presents over a wide range of age (9 to 80 years), with a slight female preponderance. Patients typically present with a slow-growing, symptom-free mass. Recurrence occurs in almost one-third of cases and there have been no reports on metastasis or mortality from these lesions [4].
SPA is a rare lesion of unknown etiology, morphologically resembling fibrocystic changes of the breast. Initially, Smith et al. [1] postulated that these lesions represent a pseudoneoplastic condition that results in both fibrosis and epithelial poliferation. However, a molecular study using the human androgen receptor assay for clonality analysis has demonstrated that this lesion is clonal and given the 30% clinical recurrence rate and hyperplastic, atypical features, SPA is a neoplasm rather than a reactive process [5].
Histologically, SPA is well-circumscribed, unencapsulated, and composed of lobules of proliferating ductules with occasional apocrine metaplasia, ductal hyperplasia, and focal cystic spaces within a dense collagenous hypocellular stroma. The glandular epithelial cells exhibit a spectrum including non-descript, apocrine, foamy vaculolated, and mucinous cells. The acinar cells often contain robust eosinophilic structures consistent with altered zymogen granules [4]. The ductal epithelial atypia, ranging from mild dysplasia to carcinoma in situ, can be found in 40%-75% of cases [6,7]. However the significance of this finding is unclear. Immunohistopathologically, luminal epithelial cells may express estrogen and progesterone receptors [7].
It is noteworthy that the eight cases analyzed by Smith et al. [1] were diagnosed initially as pleomorphic adenomas or mucoepidermoid carcinomas. The differential diagnosis includes polycystic disease, sclerosing sialadenitis, and benign and malignant glandular neoplasias. The acinar or ductal proliferation, apocrine metaplasia, and dysplasia suggest the possibility of acinar cell carcinoma, oncocytic carcinoma, or adenocarcinoma [6]. In SPA, the lobular architecture is typically maintained, the atypical nests are rimmed by myoepithelial cells, and the invasive, destructive growth pattern of a carcinoma is lacking. However, if clinicians and pathologists are not familiar with SPA, there is high chance of misdiagnosis.
Treatment for SPA is surgical excision. Recurrence occurs in almost one-third of cases and is likely due to incomplete surgical excision or multifocal disease, rather than true recurrent tumors [6]. Even through no invasive carcinoma or metastasis has been reported, if we consider that the precise nature of this uncommon lesion is unknown, it is advisable to follow patients for a long period.
In conclusion, this is the first reported case of SPA of nasal minor salivary gland origin. Although atypia ranging from mild dysplasia to carcinoma in situ can be found in some cases, SPA has a favorable outcome. Because of the infrequency of occurrence and histologic similarity of this lesion to others, it is important for otolaryngologists to familiarize themselves with SPA to reduce the likelihood of misdiagnosis.