INTRODUCTION
In onco-hematological diseases, an high incidence of rhinosinusitis is present due to alteration of the immunological asset. Moreover the increasing use of aggressive and intensive cancer chemotherapeutic regimens, immunosuppressive therapy, transplantation and radiation therapy increase dramatically the incidence of paranasal sinuses infection [1,2]. Because of their higher risk, compared to the healthy population, to develop serious complications critically ill patients with both hematological malignancies and rhinosinusitis require a timely and appropriate treatment [3,4]. Prognosis is related to various factors, such as the type of infection, the speed of diagnosis and treatment, the complete neutrophil count normalization and the involvement of structures adjacent to the site of infection as the central nervous system, the orbit and the cavernous sinus [5].
Mucositis, induced by chemotherapy treatment, leads to an alteration of mucosal defense mechanism, mucociliary clearance failure, edema, crusting and scars that can alter the sinus ostial ventilation [6,7]. Sinus dysventilation can lead to a pathological sinus cycle, the first step of rhinosinusitis.
On the other hand, surgery in this immunocompromised patients is reserved only for critical patients because of the risk of general anesthesia, infections, bleeding due to thrombocytopenia and the overall clinical state lead the surgeon to a difficult decision [8].
In traditional endoscopic sinus surgery (ESS), the combination of enlargement of sinus ostia with throughbiting instruments that incise through highly vascular sinonasal mucosa, with an inefficient haemostatic mechanisms and a lack of physiologic immune reserve, make this kind of surgery in immunocompromised and critically ill patients a challenging endeavor [9].
Dilatation surgery (DS), on the contrary, is a minimally invasive and tissue preserving procedure that relies on sinus dilation by means of inflatable balloon without mucosal cutting or removing tissue [10]. The minimally invasive nature of the technique is proposed to minimize blood loss, to induce less postoperative scarring and to facilitate the management of postoperative patient [11].
The aim of our study is to compare the surgical outcomes between traditional endoscopic and DS for the treatment of sinusitis in immunocompromised patients.
MATERIALS AND METHODS
A retrospective and non-randomized chart review was conducted in 110 patients affected by rhinosinusitis. This study was approved by the Tor Vergata Hospital Institutional Review Board and all participants signed an informed consent agreement. The patients were selected in a group of 380 hematologic patients admitted to our hospital from June 2008 to June 2012. Preoperative assessment included physical examination, sinonasal endoscopy, baseline Sino-Nasal Outcome Test (SNOT-20) calculated as the mean of the total score obtained and all patients were studied by means of computed tomography (CT) as suggested by hematology and oncology guidelines [12]. The Lund-Mackay score (Evidence Level IIb) was used for the CT disease staging. It relies on a score of 0-2 dependent upon the absence, partial or complete cloudiness of each sinus system and of the ostiomeatal complex, deriving a maximum score of 12 per side [13].
The diagnosis of rhinosinusitis was confirmed in 112 cases out of 380. Two of them presented critical general health condition, so both surgical approach was reasonable. The other 110 patients had standard indication for surgery: a strictly defined rhinosinusitis diagnosis per Rhinosinusitis Task Force criteria (symptoms including but not restricted to nasal obstruction, sinus/facial pressure, nasal discharge, and congestion) that was unresponsive to maximal medical management. Maximal medical management included three to six weeks of antibiotic therapy, inhaled and/or systemic corticosteroids, decongestants as appropriate, and saline irrigations [14].
During preoperative time 71% of patients had a platelet count <50,000 (severe thrombocytopenia), 17% 50,000-100,000 platelets (moderate thrombocytopenia), 9% 100,000-150,000 platelets (mild thrombocytopenia) and 3% had a platelet count from 150,000 to 250,000. All patients were leukopenic: 68% of them were severely neutropenic (neutrophil count <500/mmc) and the other 32% were moderate or mild neutropenic.
Patients surgically treated were subdivided in two groups: group 1 included 25 patients treated with DS since balloon was available (2008) and group 2 included 85 patients treated with ESS (Table 1). The choice of the surgical technique was based on the availability of balloon in our clinic.
All patients undergoing surgery fill out pre- and postoperative SNOT-20 surveys to determine baseline symptom status (before treatment) and improvement (if any) after intervention. The SNOT-20 rates the severity of 20 symptoms on a six-point scale (from 0 [no problem] to 5 [problem as bad as it can be]). To assess the impact of treatment, the difference between pre- and postoperative (at 3 months) SNOT-20 scores was calculated to determinate the SNOT-20 change score. At 3 month postoperative follow-up, patients underwent a global patient assessment (GPA) questionnaire to value patient satisfaction. We ask a patient to rate on a scale of +5 (the best outcome possible) to -5 (the worst outcome possible) how they feel overall; also GPA assesses patient satisfaction by asking him, if given the choice, would choose to undergo the same procedure (yes/not sure/no).
Furthermore a total symptom score was constructed (1 point for each symptom if it was present for at least 6 hours a day and affecting daily life and no points if symptom did not affect daily life or was absent). Success and improvement were defined as a decrease in the total complaint score of 1 or more points at last visit; while total improvement was defined as total resolution of all complaints (i.e., symptom score of 0).
All statistical analyses were performed using SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA). Continuous data are displayed as mean┬▒SD. Statistical significance was accepted when P<0.05. The Levine's test for equality of variances was used to determine statistically significant variances. The two independent samples test with Mann-Whitney U coefficient was used to compare the different results within each group. The Žć2 and the Fisher exact tests were used to test the association between categorical variables.
RESULTS
In 112 of 380 hematologic patients, an involvement of paranasal sinuses was present (29.4%). The infection was most common in patients with acute leukemia group compared to lymphoma or myeloma group (75 vs. 37).
Lund-Mackay scores, based on preoperative sinus CT scans, were comparable for the DS and ESS groups. P-value assessing presurgical Lund-Mackay scores between DS and ESS subjects found no significant difference (P=0.32) (Table 1).
Balloon catheters were used to treat 12 maxillary sinuses, 8 frontal sinuses, 3 sphenoid sinuses and 2 multiple sinuses. Of the 8 frontal sinuses, 3 were treated with hybrid procedure (opening of the posterior wall of the agger nasi or the anterior wall of the ethmoidal bulla) (Table 1).
In the ESS group, 40 maxillary sinuses, 27 frontal sinuses, 10 sphenoid sinuses, and 8 maxillary-sphenoid sinuses (Table 1) were treated. Local anesthesia was employed in 8 of the 25 patients (32%) treated with DS and in 15 of the 85 patients treated with ESS (17.6%). General anesthesia was necessary in the others 17 patients treated with DS and the 70 patients treated with ESS (P=0.123) (Table 1).
No major adverse events were reported linked to th surgery techniques. In 50 ESS patients group treated an anterior nasal packing was placed at the end of the procedure and in 12 patient with a minor bleeding a new anterior nasal packing was necessary after 4 days. In the DS group nasal packing was required in 8 cases and in 2 cases a repacking was necessary (P=0.019 and P=0.422, respectively) (Table 1). A postoperative nasal debridement was necessary in 25 patients of ESS group and in 3 of DS group (P=0.08).
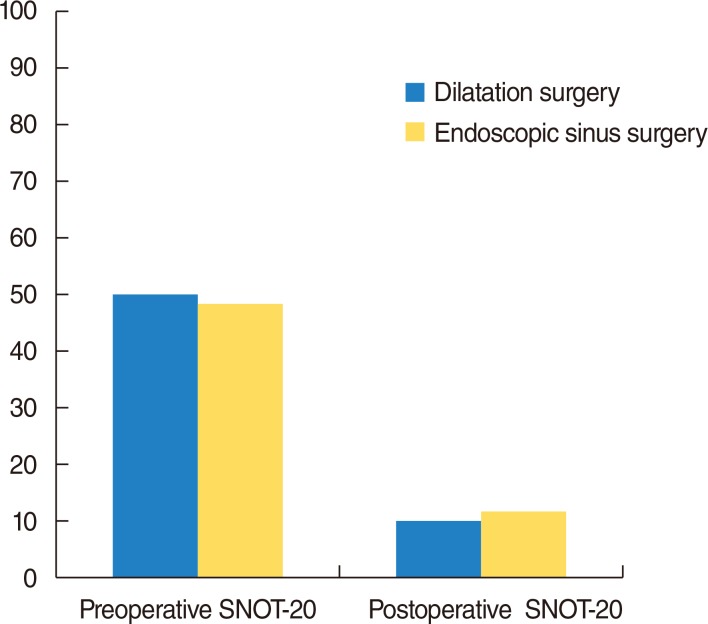
The t-test analysis revealed improvement in SNOT-20 scores following surgery in both dilatation and ESS group (P<0.001). The preoperative SNOT-20 scores were 58┬▒10.4 in DS patients and 56┬▒17 in patients treated with ESS, showing well-matched group. The mean 3-month postoperative SNOT-20 scores after DS (17.6┬▒11) was less than ESS postoperative SNOT-20 scores (19.6┬▒17.4). The SNOT-20 different score of both procedures showed clinically significant improvement of health status: 39.8┬▒13.2 for DS group and 36.2┬▒19.6 for ESS group. But also an improvement was recorded the DS group in 3 voices of SNOT-20: need to blow nose, runny nose, and facial pain/pressure (Fig. 1).
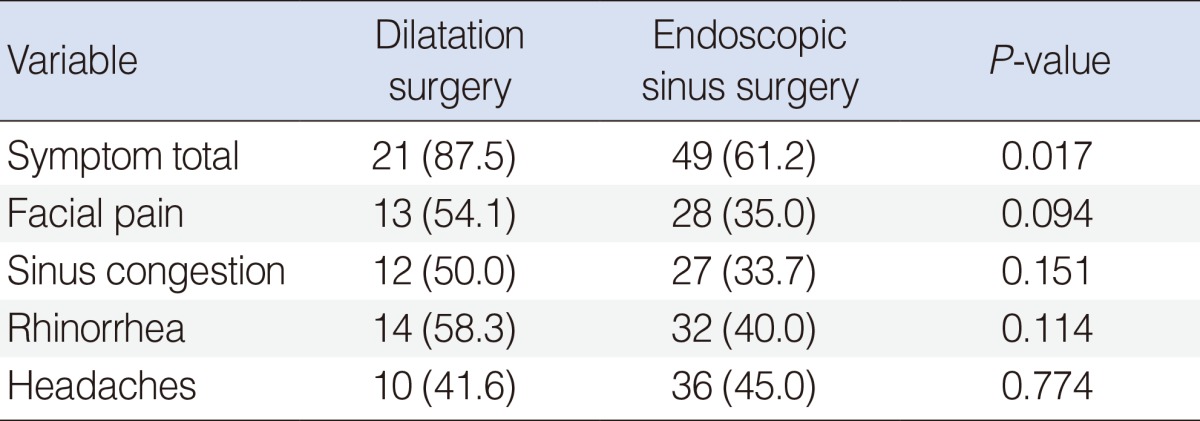
Table 2 is showed the overall improvement in reports of specific preoperative symptoms at final postsurgical visit as measured at 3 month postsurgical follow-up. Both group had improvement of symptoms during the follow-up period. 87.5% of patients who underwent DS and 61.2% of patients who underwent ESS demonstrated a reduction of symptoms at 3 month postoperative follow-up (P=0.017) (Table 2).
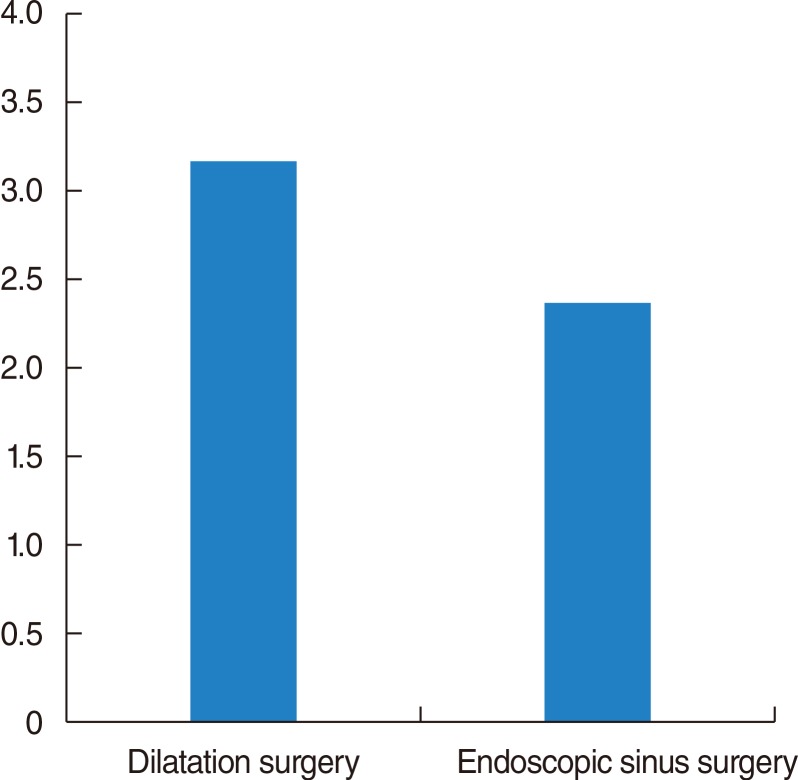
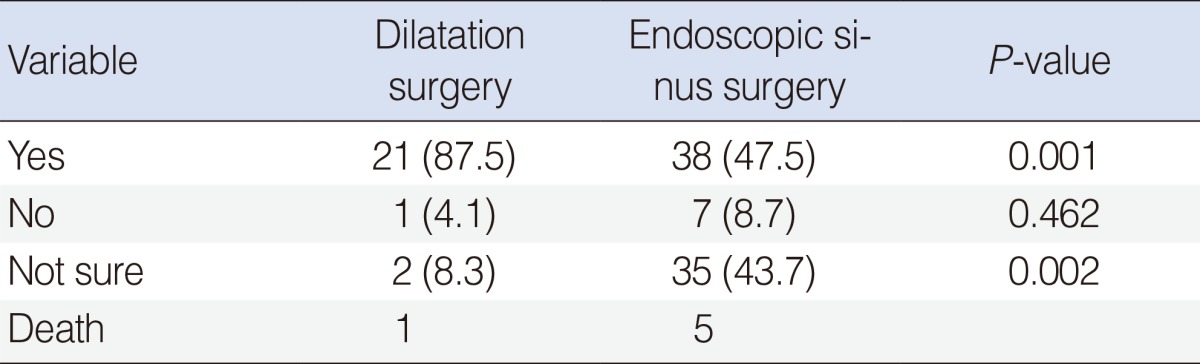
The 3-month follow-up GPA form questionnaire recorded that 87.5% of DS patients responded with "yes" to having the same procedure done again, instead only 47.5% of post-ESS patients said "yes" (P=0.001) (Table 3). Additionally, 4.1% of DS patients responded with "no" and 8.3% were "not sure" when faced with the same question, versus 8.7% and 43.7% of the post-ESS patients, respectively (P=0.462 and P=0.002, respectively) (Table 3, Fig. 2).
DISCUSSION
In the last 20 years, as results of improved imaging and surgical techniques, sinus surgery has become more conservative [15,16]. To date ESS is the optimal surgical procedure for patients affected by sinusitis who not responding to medical management. A success rates between 75% and 95% is typically reported [17]. However major complications still occur in approximately 1.1% of surgery and minor complications, including bleeding, infection, periorbital emphysema, ecchymosis and synechiae, occur in 5.4% of cases [18]. The technical philosophy of ESS includes enlargement of sinus ostia and elimination of the surrounding mucosal contact areas. A constant growth of technical development has been a drive toward more delicate instrumentation that could help the surgeon to respect nasal mucosa. An enlargement of the surgical armamentarium was obtained introducing the DS tool.
This minimally invasive surgical procedure is able to dilate the sinus ostia preserving mucosa and saving the mucociliary transport function [19]. DS is a complementary tool for endoscopic nasal surgery and it is usually employed only in isolated sinusitis. In immunocompromised patients, DS seems to obtain multiple advantages and some remarks can be drawn.
In a critical mucosal condition, the intraoperative blood loss is insignificant. The lower number of anterior nasal packing and repacking confirm the low aggressiveness of the procedure. As a consequence, the development of crusting and synechiae is lower and postsurgical nasal debriment is necessary in a reduced number of patients. This is a very important goal since the general condition of these patients are often poor and any medical invasive treatment should be avoided.
Local anesthesia was possible in a larger group of DS patients, although the higher complexity surgical procedure were performed in ESS group. All these remarks may lead the surgeon to consider a large number of candidates for this surgical procedure.
A balance between the surgery and the natural evolution of the paranasal infection is mandatory to prevent the critical evolution of the infective disease. A rapid spreading of the infective disease through the surrounding tissue lead to an aggressive paranasal surgery. Probably, the use of DS could avoid the progressive clinical distrectual worsening. DS allows to act timely on a damaged mucosa because of chemotherapy treatment. As a consequence, the restored mucociliary clearance led to a normal sinus cycle re-establishing the physiological sinus ventilation and arresting disease progression in immunocompromised patients.
In according with other authors, we demonstrated the efficacy of balloon sinuplasty as non inferior to ESS in treatment of rhinosinusitis [20]. Our results prove the safety and feasibility of this surgical procedure yet established in previous studies [13,21,22,23,24,25]. However we demonstrate the safety and efficacy of this technique also in onco-hematological patients with sinus dysfunction. In literature there is only one study analyzing the balloon sinuplasty technique in 5 immunocompromised patients [9]. All underwent sinus surgery with no complication, minimal blood loss, and no need for transfusion. To our knowledge only a case of surgical complications in hematological patients is reported: a septal hematoma, spontaneously resolved was descripted after dilatation of the sphenoid natural ostium by means of balloon [26,27].
DS represents a potentially low aggressive treatment and appears to be relatively safe, effective in onco-hematologic patients, minimizing mucosal and structural damage, period of healing and postoperative debridements.
Patients affected by hematological cancers showing an infectious involvement of the paranasal sinuses have a substantially higher risk than the general population to suffer from serious local and systemic complications. Therefore a timely medical and surgical treatment is necessary. DS represents a potentially low aggressive technique and appears to be relatively safe, effective and feasible, as demonstrated by procedural technical success, patient tolerability, and clinical outcomes. Minimizing mucosal and structural damage, period of healing, postoperative debridements and using local anesthesia it should be considered a valid option in onco-hematologic patients.