INTRODUCTION
Even though laryngotracheal strictures that are due to inhalation injuries frequently occur, the current treatment options for this medical condition are limited. The management of laryngotracheal strictures that are caused by damage to the tracheal tissue from heat and intubation remains challenging. The acute treatment goal is preservation of airway access, while the later treatment focuses on restoring a proper laryngotracheal lumen (1).
Slide tracheoplasty has several advantages for reconstructing a stenotic segment of the trachea, and especially in children with congenital long-segment tracheal stenosis. The primary advantage of this technique is reduction of the tension on the anastomosis; this alleviation of pressure is obtained by reducing the approximation distance. Furthermore, the vascularity of the tracheal cartilage is preserved, and this allows for better healing. A few articles have recently suggested that slide tracheoplasty could be a useful method for treating upper tracheal stenosis in adults (2-4).
We report here on a case of a patient who had recurrent upper tracheal stenosis after an inhalation injury. Repetitive symptoms of stenosis were present even after balloon dilatation, several bouts of laryngomicrosurgery (LMS) and resection with end-to-end anastomosis surgery. We then successfully treated the stenosis by performing slide tracheoplasty.
CASE REPORT
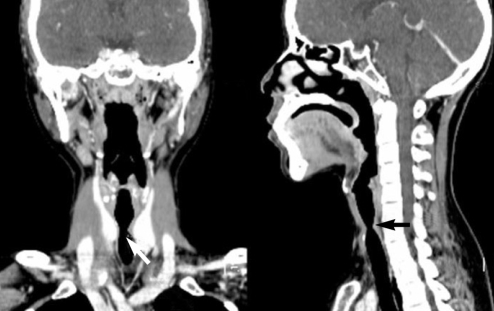
A 31-yr-old female visited our department in October 2002. She had a history of endotracheal intubation for a week to maintain her airway after an inhalation burn, and she then developed dyspnea after the treatment. Prior to the inhalation injury, she had no family history of disease or any notable medical conditions. On physical examination, the mobility of both vocal folds was found to be intact; however, we observed upper tracheal stenosis. The patient's airway was severely compromised with less than 30% of the normal function due to the stenosis. A neck computed tomography (CT) scan showed a tracheal stenosis lesion around the 6th cervical spinal level. The narrowest diameter of the lesional trachea was about 0.7 cm and the lesion length was about 3cm. Slight enhancement was also visible on the stenotic lesion, which most likely due to granulation tissue. We performed bronchoscopy and balloon dilatation procedures. The 10 mm balloon dilatation was initially successful, but further procedures could not be performed because of the patient's unstable vital signs. We decided to perform a resection with end-to-end anastomosis in November 2002. We performed a hyoid release and resection of a 2 cm segment of the trachea (from the 2nd to 5th tracheal rings) 2 months after the burn injury. Two months later, the dyspnea symptoms reappeared and the tracheal stenosis was found. Tracheal ballooning and stent insertion were then performed, but the stent was removed after 1 month due to displacement. Granulation tissue was observed a few months later at the previous operative site. LMS was performed next to remove the granulation tissue and mitomycin C was applied. In 2006, upper tracheal stenosis due to a fibrous stricture of the tracheal mucosa was found. A neck CT scan revealed a narrowed airway with hour-glass-shaped tracheal rings on the 6th cervical spinal level (Fig. 1). The narrowest diameter of the trachea was about 0.6-0.7 cm and LMS then was performed two more times. Five years after the inhalation injury, we performed slide tracheoplasty to treat the stenotic tracheal lesion.
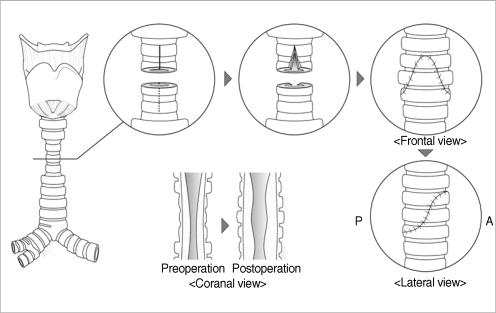
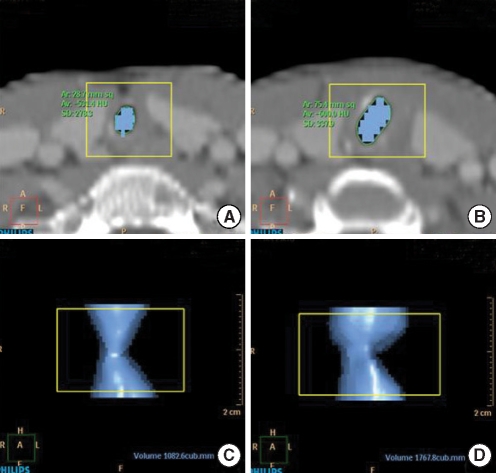
The procedure was performed under general anesthesia and the airway was secured using an endotracheal tube. A transverse midline neck incision along with a thyroid split was performed. Additional dissection was performed 4 to 5 cm distal to the site of the stenosis. The dissection was meticulously performed to avoid damage to the recurrent laryngeal nerves. Three circumferential narrowed tracheal rings were observed, and transection of the stenotic trachea was performed at the narrowest midpoint; thick fibrous mucosal changes were observed. The proximal half of the trachea was split along its anterior wall, while the distal segment was split along its posterior wall. The right angle corners, where the vertical incisions met the transverse incision, were trimmed. Both ends of the trachea were then anastomosed (Fig. 2). The endotracheal tube was advanced to the distal area of the reconstruction. Extubation was done on postoperative day 2. On postoperative day 7, we confirmed that the anastomosis site was healing and that the upper tracheal lumen was maintained with about 70% patency by a telescopy-guided examination. Three months after the operation, the tracheal anastomosis area was visually healthy and the upper trachea was enlarged. A follow-up neck CT scan revealed a more widened tracheal lumen. Objective improvement of the airway was confirmed on the CT image with using a 3D volume rendering technique at the levels 15 mm above and below the stenosis area. The preoperative selected airway volume of 1,082.6 mm3 had increased to 1,767.8 mm3 postoperatively (Fig. 3). The patient has been followed up for 18 months and there has been no tracheal narrowing or symptoms of dyspnea.
DISCUSSION
Acquired tracheal stenosis is a fibroproliferative disorder. Various factors can cause tracheal stenosis, including prolonged endotracheal intubation, severe inflammation, autoimmune disorders, iatrogenic disorders and inhalation burns. Many factors can adversely affect a tracheal stenosis and increase the growth of granulation tissue in patients suffering with inhalation burns. The initial insults caused by an inhalation injury can resolve easily if no airway stricture is present; however, if a transmural injury initially occurs or it occurs as a consequence of additional trauma caused by intubation, then granulation and scar tissue formation may occur, leading to stenosis (1, 5, 6). The duration of the intubation and the motion of the intubation tube caused by the ventilator are also possible reasons why stenosis might occur. Tracheal infection can also inhibit wound healing, causing granulation tissue to form as a result of an abnormal healing process; this tissue can eventually develop into a stenosis (7). In most patients, the tracheal inflammation subsides over a period of 3 to 5 yr, and the granulation tissue on the tracheal wall becomes firm. Even though the optimal time for resection of a tracheal stenosis is unclear, delayed repair is recommended for fewer recurrences (2). We performed resection with end-to-end anastomosis surgery 2 months after the burn. It is possible that at this time point, the granulation tissue was still friable and that it still had great proliferative potential. These may be the main reasons for the failure of the resection with performing end-to-end anastomosis surgery. Another possible reason for the failure may have been the presence of the narrow, hourglass-shaped airway and tracheal rings. Schweizer et al. (8) mentioned that tension may tear an anastomosis, which is the weakest part of the trachea, resulting in an hour-glass shape after end-to-end anastomosis surgery (8, 9).
Management of tracheal stenosis is challenging because of the high incidence of restenosis. Selection of the type of treatment depends on the patient's clinical status and the anatomical pattern of the stenosis. The technique of slide tracheoplasty was developed to repair supracarinal long-segment tracheal stenosis. This technique includes transecting the trachea in the mid-stenosis and performing an oblique side-to-side anastomosis (10). This reduces the tracheal length, but it doubles the circumference, quadruples the cross-sectional area and decreases the resistance to airflow. In addition, this technique prevents the risk of circular shrinking. Slide tracheoplasty with limited resection can prevent such complications. This technique can be used for the management of acquired subglottic and upper tracheal stenosis with a relatively long segment (2-4). In our case, the patient had already undergone resection with end-to-end anastomosis surgery and we could not perform that surgery again because her trachea was too short at this stage. So we considered slide tracheoplasty a valid treatment option. The surgery was completed successfully and the patient's postoperative checkup-findings and telescopy-guided examination indicated that the patient's airway volume had increased as a result of the slide tracheoplasty.
In conclusion, even though the optimal time for performing resection of a tracheal stenosis in inhalation burn patients is unclear, delaying the surgery for an appropriate period of time is important for fewer recurrences. Slide tracheoplasty is a safe, effective procedure that can be used to successfully treat problematic recurrent stenotic upper tracheal lesions, and even in patients with a trachea that has been shortened by resection with end-to-end anastomosis.