Modified Transoral Endoscopic Thyroidectomy Technique Using Trapdoor Suspension Sutures
Article information
Transcervical thyroidectomy has been the standard operative method, but it leaves a permanently visible scar in the anterior cervical region. Various remote-access thyroidectomy techniques [1] have been developed to hide this scar, but these techniques involve some risks and limitations, including extensive dissection, increased likelihood of nerve and vascular damage, and a narrow and deep working space [2,3]. Recently, the transoral endoscopic thyroidectomy vestibular approach (TOETVA) technique has been developed and refined by Anuwong et al. [4,5] to minimize dissection distance and the likelihood of nerve damage. However, this approach might have several complications, such as CO2 embolism and subcutaneous emphysema, if CO2 is continuously insufflated to expand the operation field [6,7].
In an effort to address these problems, we developed a new approach for TOETVA, which we refer to as modified transoral endoscopic thyroidectomy using trapdoor suspension sutures. We employed transoral endoscopic thyroidectomy without CO2 insufflation to obviate the risk of fatal complications such as CO2 embolism. We also did not use a retractor because of the possibility of facial sensory numbness and instrument interference. Herein, we present a case series of our early experiences with this technique to evaluate its feasibility, usefulness, and safety in properly selected patients.
The authors obtained approval from the Institutional Review Board of Kyung Hee University Medical Center (IRB No. KHUH 2020-12-010). A retrospective analysis was conducted of patients who underwent modified transoral endoscopic thyroidectomy using trapdoor suspension sutures by a single surgeon. Patients were selected for modified transoral endoscopic thyroidectomy based on the guidelines proposed by Tae et al. [8]. Demographic characteristics, clinical features, pathological status, surgical details, complications, and cosmetic satisfaction were analyzed. Facial sensory numbness was checked at 2 and 4 weeks after operation at five sites: the middle mentum, right mentum, left mentum, submentum, and lower lip. Sensory numbness was evaluated on a scale of 0 (no sensory) to 10 (normal) using a questionnaire.
The surgical procedures were conducted similarly to previous studies [5,8], except that we used multiple trapdoor sutures and an L-shaped suspension bar instead of using CO2 gas and a retractor. Briefly, a 10-mm 0° laparoscope was placed in a 10-mm trocar inserted into a vestibular midline transverse incision. An external trapdoor silk 2-0 suture using a reverse cutting needle was placed in the anterior midline of the neck to elevate the subplatysmal flap and retracted using an L-shaped suspension bar. The needle was inserted from the outside of the skin where the endoscopic light shone, grasped by needle forceps, and then passed through the contralateral skin again to perform trapdoor sutures. The subplatysmal working space was made by dissection with an ultrasonic device, L-hook cautery, and laparoscopic instruments. After changing the 0° laparoscope to a 30° laparoscope, a skin flap was elevated to the level of the sternal notch inferiorly and to the edge of the sternocleidomastoid muscle laterally. The dissected subplatysmal flap was retracted by multiple external trapdoor sutures and the L-shaped suspension bar (Fig. 1A). The midline raphe between the strap muscles was identified and divided. The divided strap muscles were dissected from the ipsilateral thyroid lobe, and the entire anatomy of the anterior neck area was well exposed to a degree similar to that of standard TOETVA via CO2 insufflation (Fig. 1B) [5]. Thyroidectomy was conducted as described in previous studies [5,8].
External and endoscopic findings in modified transoral endoscopic thyroidectomy using trapdoor suspension sutures. (A) Multiple external trapdoor sutures were hung on an L-shaped suspension bar using hemostatic forcep. (B) Exposure of the anterior neck area using a 30° laparoscope.
Eight patients (1 man and 7 women) underwent modified transoral endoscopic thyroidectomy using trapdoor suspension sutures (mean age, 41.75±13.68 years). The clinicopathological features of these eight patients are summarized in the order of surgery, as shown in Supplementary Table 1. Six patients were diagnosed with papillary thyroid carcinoma (PTC) and two patients were diagnosed with nodular hyperplasia using sonography-guided fine-needle aspiration. The extent of operation was lobectomy with isthmusectomy in PTC patients and isthmusectomy in patients with nodular hyperplasia confined to the isthmus.
The mean operation time was 196.67±58.74 minutes for lobectomy with isthmusectomy (Table 1). However, there was a steep learning curve, and the operation time reached 132.00 minutes for our sixth lobectomy and isthmusectomy case. This might have been because of acclimation to the setting process and the use of more selective indications. As cases continued, the thyroidectomy time decreased significantly. The mean operation time for only isthmusectomy was 94.00±5.66 minutes. This suggests that isthmusectomy is a good indication for transoral endoscopic thyroidectomy without CO2 gas or a retractor.
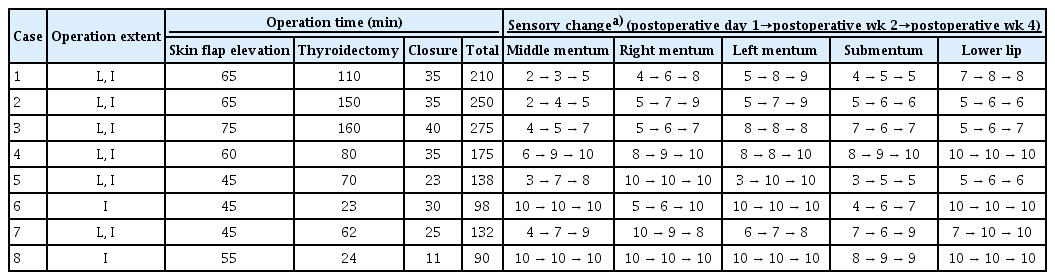
Operation time and sensory changes of eight patients treated by modified transoral endoscopic thyroidectomy using trapdoor suspension sutures
Modified transoral endoscopic thyroidectomy has similar advantages to standard TOETVA via CO2 insufflation. Additionally, there is no risk of severe complications such as CO2 embolism when using the modified technique. However, using the modified technique, it takes longer to perform subplatysmal dissection from the mouth to the sternal notch than in the standard TOETVA technique using CO2 insufflation.
There were no postoperative complications, including recurrent laryngeal nerve palsy, hematoma, seroma, infection, or tracheoesophageal injury. Hypoparathyroidism was not evaluated because we did not perform total thyroidectomy. Unlike transcervical thyroidectomy, complications such as skin flap perforation, mental nerve palsy, and facial sensory numbness may arise in transoral endoscopic thyroidectomy. There is no platysma muscle in the midline neck area. Thus, special attention is required not to puncture or burn the anterior neck skin. Mental nerve injury was prevented by taking a panoramic view and confirming the location of the mental foramen. Facial sensory numbness was our special area of interest. The first two patients complained of transient middle mentum numbness, although sensation recovered to some extent after 4 weeks (Table 1). This might have been due to a sustained retraction and a long operation time during our learning curve. Thus, we intermittently released the external trapdoor sutures to relieve sustained and excessive retraction. Subsequently, patients did not complain about severe facial sensory numbness on the first day after the operation. We also evaluated postoperative cosmetic satisfaction. Only external trapdoor suture points were visible after 1 day and 2 weeks later. Four weeks later, most suture points had disappeared. All patients were very satisfied or satisfied with their cosmetic status at 4 weeks after the operation.
However, the indications for transoral endoscopic thyroidectomy are limited compared to transcervical thyroidectomy, especially in the initial phase of implementation. Tae et al. [8] stated that the ideal indication for TOETVA might be a benign and differentiated thyroid tumor <2 cm in diameter not located in the uppermost part. We selected patients relatively strictly by referring to the above indications because these were our initial experiences in modified transoral endoscopic thyroidectomy using trapdoor suspension sutures. Thus, this study has a small sample size limited to a restricted group of patients. The indications can be expanded in the future as we continue to perform this procedure.
In conclusion, our institution has successfully implemented modified transoral endoscopic thyroidectomy using trapdoor suspension sutures for thyroid surgery in selected patients. Based on our initial experiences, transoral endoscopic thyroidectomy without CO2 gas or a retractor is a safe and feasible method showing excellent cosmetic outcomes when it is applied to patients with appropriate indications. Further experiences are needed to evaluate the indications, feasibility, and safety of this technique in more detail.
Notes
No potential conflict of interest relevant to this article was reported.
Acknowledgements
This work was supported by a National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) (No. 2020R1A5A201941311).
Notes
AUTHOR CONTRIBUTIONS
Conceptualization: SIK, YGE, SGK. Data curation: HKM, DWK, SYC, HJK. Formal analysis: SIK, YCL, YGE, SGK. Funding acquisition: YGE, SGK. Methodology: all authors. Project administration: YCL, YGE, SGK. Visualization: SIK, HKM, DWK, SYC, HJK. Writing–original draft: SIK, YGE. Writing–review & editing: all authors.
Supplementary Materials
Supplementary materials can be found via https://doi.org/10.21053/ceo.2021.00101.
Clinicopathological summary of eight patients treated by modified transoral endoscopic thyroidectomy using trapdoor suspension sutures
