 |
 |
- Search
AbstractObjectivesThis study aimed to evaluate long-term changes after balloon dilation of the Eustachian tube (BDET) in chronic otitis media (COM) patients with Eustachian tube (ET) dysfunction that persisted after tympanomastoidectomy (TM).
MethodsWe retrospectively reviewed the medical records of consecutive patients who were diagnosed with COM and ET dysfunction and underwent TM at our tertiary hospital from 2016 to 2017. The tympanic membrane status, the presence of a ventilation tube, ability to perform the Valsalva maneuver, and audiologic changes after dilation of the ET were analyzed.
ResultsThis study included 20 patients (with 21 ears) who underwent TM but could not perform the Valsalva maneuver, showed a persistent air-bone gap, and eventually underwent BDET (male:female, 8:13; right:left, 11:10). Four ears showed perforation of the tympanic membrane after TM. Among the remaining 17 ears, 15 ears underwent ventilation tube insertion before BDET, while two ears underwent ventilation tube insertion and BDET simultaneously. Although none of the patients were capable of the Valsalva maneuver before BDET, 13 (62%) were able to perform the Valsalva maneuver successfully after BDET. When evaluating the tympanic membrane status at the latest follow-up, ventilation tubes were still present in eight ears. In the other 13 ears, intact tympanic membranes were present in nine out of 11 ears n the successful Valsalva group, whereas none of them were intact in the unsuccessful Valsalva group (P=0.014). The successful Valsalva group after BDET showed an improved air-bone gap of 8.9±12.4 dB, while the unsuccessful Valsalva group showed an aggravated air-bone gap of 3.8±11.8 dB at 1 year after BDET; this difference was statistically significant (P=0.031).
Chronic otitis media (COM) refers to an inflammatory condition of the middle ear lasting for at least 3 months. Although some studies have argued that Eustachian tube (ET) dysfunction is not a leading cause of COM [1,2], many studies have supported the hypothesis that dysfunction of the ET plays an important role in the etiology of COM [3,4]. The major functions of the ET are equalizing the pressure, facilitating the mucociliary clearance of secretions, and protecting the middle ear [5]. When the ET does not work properly, negative pressure in the middle ear accumulates, which can lead to the retraction of the tympanic membrane and fluid accumulation in the middle ear [5,6], resulting in COM.
Medical treatment, including nasal steroids, decongestants, and antihistamines, has been empirically tried to improve the mucosal conditions of the nasal cavity and ET. More invasive treatments have also been tried, such as paracentesis and the insertion of ventilation tubes to equalize pressure via the tympanic membrane [7,8]. However, these approaches could not solve the dysfunction of the ET in a direct way [9]. Surgical widening of the cartilaginous ET using a laser or microdebrider has been attempted for opening the ET with limited success [10,11]. Thus, no definite treatment for ET dysfunction emerged until balloon dilation of ET (BDET) was introduced in 2010 [9,12,13]. In this technique, a balloon is directly placed in the cartilaginous ET and inflated to mechanically dilate the cartilaginous part of the ET [9]. This procedure resulted in improved ET function in 66%–100% of patients and a reduction in symptoms [14]. Despite these successful results of BDET, there are still some cases of failure even with repeated BDET, and stent insertion into the cartilaginous ET is under development to treat these failure cases [15,16].
Although the dysfunction of the ET plays an important role in the etiology of COM, there have been few studies that evaluated the efficacy of BDET in patients with COM. As summarized in a review article [14], most studies reported short-term changes after BDET and the majority of studies regarding BDET focused on otitis media with effusion. Since some COM patients have underlying problems related to ET dysfunction, some COM patients with ET dysfunction will still need treatment for ET dysfunction even after successful ear surgery. Therefore, this study aimed to identify the ability to perform the Valsalva maneuver successfully, long-term changes in hearing thresholds, and the status of the tympanic membrane in COM patients with persistent ET dysfunction who underwent BDET after tympanomastoidectomy (TM).
A retrospective analysis of the medical records was conducted for consecutive patients who underwent BDET after TM from January 2016 to December 2017 at a single tertiary medical center. Any patients who underwent TM were asked to perform a Valsalva maneuver, starting from 3 to 4 weeks after surgery. The entire packing in the external auditory canal was removed under the microscope at 2 weeks after TM. Gelfoam pledgets filling the canal were removed by gentle aspiration using the smallest possible suction tubes. Otic drop was applied and the canal was cleaned regularly for 1–2 additional weeks. And then, the patient was instructed to perform a Valsalva maneuver when the fascia looked well attached under the endoscope. Thus, any patients who underwent TM were asked to perform a Valsalva maneuver regularly (every hour, 10 times a day) at 3–4 weeks after the surgery. They were instructed to hold their breath by increasing the pressure for 5 seconds repeatedly until they felt any pressure change in the operated ear. They were instructed not to do a Valsalva maneuver further if they feel pressure changes in the ear, because too much inflation might rupture the tympanic membrane in the early postoperative stage. Successful Valsalva maneuver was defined positive, when the bulging of the tympanic membrane could be observed by endoscopic examination or a patient felt the air passage when there was a perforation of the tympanic membrane (or ventilation tube was in place), while the patients were asked to do a Valsalva maneuver. When a patient could do a Valsalva maneuver successfully, he/she was followed up 6 months later, otherwise he/she was instructed to perform the Valsalva maneuver regularly (every hour, 10 times a day) and scheduled to visit an outpatient clinic 2–3 weeks later.
When patients could not perform a Valsalva maneuver even after 2–3 weeks of Valsalva trial period and there was also a persistent air-bone gap in pure-tone audiometry, they became a candidate for BDET. A ventilation tube was inserted to the tympanic membrane for immediate resolution of the middle ear effusion before BDET or simultaneously with BDET. When patients could not perform a Valsalva maneuver even after 2–3 weeks of Valsalva trial period and there was also a persistent airbone gap in pure-tone audiometry, they became a candidate for BDET. A ventilation tube was inserted to the tympanic membrane for immediate resolution of the middle ear effusion before BDET or simultaneously with BDET. After BDET, the patients were asked to do a Valsalva maneuver more than ten times per day from the day after the procedure and were followed up at 1 week, 3 months, 1 year and as needed postoperatively.
The study protocol of this study was approved by the Institutional Review Board of Asan Medical Center (No. 2019-0863) and written informed consents were obtained from all patients.
Hearing thresholds was determined by pure tone audiometry (PTA), and the mean hearing levels were expressed as the average of the hearing thresholds at 0.5, 1, 2, and 4 kHz (four-frequency average). All patients were evaluated by PTA prior to BDET and at 3 months and at least yearly after dilation. The air-bone gap was measured before and after BDET.
All patients underwent topical anesthesia by placing surgical sponges soaked with normal saline containing 4% lidocaine and 1:1,000 epinephrine to the nasal cavity and on the nasopharyngeal opening of ET for 5 minutes. A metallic guide sheath, a 0.035‐inch flexible guidewire (Radifocus M; Terumo, Tokyo, Japan) and a 6‐mm wide, 20‐mm long balloon catheter (Genoss Co. Ltd., Suwon, Korea) were used. With endoscopic guidance, the guiding sheath was advanced through the nasal cavity to the orifice of the ET (Fig. 1A). The guidewire was then introduced through the cartilaginous ET into the bony ET via fluoroscopic guidance (Fig. 1B). And then the balloon catheter was passed through the inserted guidewire until it reached the first mild resistance approaching the narrowest diameter before the bony‐ cartilaginous isthmus. All procedures were performed in the Hirtz position for a submento‐vertical view to identify both the location of the guidewire and the inflation of the balloon catheter under fluoroscopic guidance (Fig. 1C) [17]. The balloon was then inflated with water‐soluble contrast medium (Omnipaque 300; GE Healthcare, Cork, Ireland) to reach 10 atm for 1 minute and then deflated. And the balloon catheter was inserted deeper until it reached mild resistance and inflated again for another 1 minute.
Patient demographic and clinical data were collected, including age, sex, side, chief complaint, mean follow-up period, the status of the tympanic membrane, and the presence of a ventilation tube. The ability to perform a Valsalva maneuver and any audiology changes were evaluated. The latest tympanic membrane status was also evaluated and compared between the successful and unsuccessful Valsalva groups.
Continuous variables are expressed as mean and standard deviation or median and range, while categorical variables are expressed as the number and percentage. Variables were compared using Mann-Whitney U-test, chi-square test or Fisher’s exact test. A P-value of less than 0.05 was considered significant. Statistical analyses were performed using IBM SPSS ver. 24.0 (IBM Corp., Armonk, NY, USA).
During the study period, 20 patients (13 men and 8 women, aged from 31 to 71 years old, with 21 ears), were enrolled in this study. The mean follow-up period was 69 months (range, 9–238 months). Patients’ demographic characteristics are summarized in Table 1. There was no significant difference between ears on the left and right side. The most common chief complaints were hearing disturbance (57.1%), followed by ear fullness (28.6%), otorrhea (9.5%), and tinnitus (4.8%). Canal wallup mastoidectomy was performed in 13 ears (61.9%), while canal wall-down mastoidectomy was performed in eight ears (38.1%).
No patients could perform the Valsalva maneuver successfully with a persistent air-bone gap after TM, but they could perform the Valsalva maneuver successfully on the non-operated ear except for one patient who showed bilateral ET dysfunction. After BDET, it was possible for patients to perform the Valsalva maneuver successfully for 13 (61.9%) of the 21 ears at the 1-year follow-up and for 10 (47.6%) of the 21 ears at the latest follow up. Among 21 ears, 17 ears required ventilation tube insertion before or simultaneously with BDET. The other four ears already had tympanic perforation, and therefore ventilation tube insertion was not required.
After BDET, the tympanic membrane was evaluated according to the ability to perform the Valsalva maneuver at the last follow-up (Table 2). Eight ears still had the ventilation tube inserted at the latest follow-up. Six of them were included in the unsuccessful Valsalva group and needed the ventilation tube for tympanic aeration. The ventilation tube was present in two ears in the successful Valsalva group because it was left in place until it spontaneously fell out in that group. Nine of the successful Valsalva ears had an intact tympanic membrane, whereas two ears had an abnormal tympanic membrane; there was one case of retraction and one case of perforation. Among the unsuccessful Valsalva ears, two ears had an abnormal tympanic membrane, with one case of retraction and one case of perforation. In summary, the ears in the successful Valsalva group showed normal tympanic membranes more frequently than those in the unsuccessful Valsalva group (P=0.014).
Fig. 2 shows the individual-level hearing outcomes of the airbone gap before and 1 year after BDET. Fig. 3 shows changes in the air-bone gap after DBET in the successful and unsuccessful Valsalva groups. The air-bone gap improved by 8.9±12.4 dB when comparing pre-BDET and 1 year post-BDET in the successful Valsalva group, while the unsuccessful Valsalva group had a decreased air-bone gap of 3.8±11.8 dB. This difference was statistically significant (P=0.031). When comparing the pre-BDET findings and the latest results, hearing improvement was observed in the successful Valsalva group (5.4±9.3 dB), whereas a decrease was observed in the unsuccessful Valsalva group (0.8±11.6 dB); however, the difference was not statistically significant (P=0.584).
Several plausible medical and surgical treatment options, such as a ventilation tube, for ET dysfunction have been introduced [7-11], but they could not solve the ET dysfunction itself. BDET was introduced to address cases where other treatment options for ET dysfunction are ineffective [9]. Previous cadaveric and numerous clinical studies proved the safety and effectiveness of BDET [13,18-26]. These successful results were also observed in children. A study reported that BDET effectively improved audiologic outcomes by decreasing the air-bone gap compared to ventilation tube insertion alone for otitis media with effusion in children [27]. Another study also reported the safety and efficacy of BDET for obstructive ET dysfunction in children [28]. Although most studies used endoscopy-guided BDET, endoscopy and fluoroscopy-guided balloon dilation of the ET was also successfully introduced without major complications [29,30]. Another study demonstrated that a low pressure during balloon dilation was sufficient to inflate the balloon via fluoroscopic guidance, suggesting that an excessively high inflation pressure is not needed [31]. We used a 6-mm-wide by 20-mm-long balloon catheter and the balloon was inflated at 10 atm. Two balloon dilation systems are widely available; the Bielefeld system inflates the balloon at 10 atm for 2 minutes, whereas the Acclarent system does so at 12 atm for between 30 seconds and 2 minutes [31]. In the Bielefeld system, the balloon is 20 mm long with a diameter of 3.28 mm, and thus has a smaller diameter than either the Acclarent system or the balloon we used here. The Acclarent balloon is 16 mm long with a diameter of 5 or 7 mm. Although it is challenging to compare the effectiveness of different systems, the reported efficacies of the Bielefeld and Acclarent balloons seem to be comparable [21,23,32].
Our results showed that the Valsalva maneuver could be performed successfully after endoscopy- and fluoroscopy-guided ET balloon dilation in 62% of patients with COM who underwent TM but still had ET dysfunction. Moreover, this technique enabled more frequent preservation of an intact tympanic membrane by making aeration of the tympanic cavity possible. An improved air-bone gap after BDET was also observed at 1-year follow-up after BDET.
Most previous studies analyzed the clinical outcomes of BDET in patients with middle ear effusion. Although the dysfunction of the ET plays an important role in the etiology of COM [3,4], few studies have evaluated the efficacy of BDET in patients with COM. A recent study demonstrated the BDET with ventilation tube insertion effectively improved the symptoms and the ET score in adults with recurrent COM [33]. Since there is a lack of studies regarding the effects of BDET in patients with COM, our study is meaningful in that it focused on the effects of BDET on clinical features, as well as the audiologic differences between patients with COM who could or could not perform the Valsalva maneuver.
The capability to perform the Valsalva maneuver represents adequate functioning of ET for middle ear ventilation by performing moderately forceful attempted exhalation against a closed airway. After mechanical dilation of the ET, airflow can be detected subjectively and objectively in the middle ear from the ET orifice opening in the nasopharynx when performing the Valsalva maneuver, whereas this could not be observed before BDET. This can be an initial step towards solving problems in the middle ear. With aeration in the middle ear, this study demonstrated that COM patients who could successfully perform the Valsalva maneuver after BDET could maintain good tympanic aeration and an intact tympanic membrane, and eventually have better hearing than those who could not.
This study has several limitations. First, most COM patients could perform the Valsalva maneuver successfully, suggesting that ET dysfunction might have been present only when it had caused COM. Therefore, this study does not support the generalization that all COM patients have ET dysfunction; instead, it implies that BDET can be conducted for COM patients with persistent ET dysfunction after TM. Secondly, an inability to perform the Valsalva maneuver does not always mean that ET dysfunction is present, because even normal subjects can perform the Valsalva maneuver only 78%–86% of the time [34]. For this reason, we performed BDET only for the COM patients who could not perform the Valsalva maneuver and had a persistent air-bone gap, which might also be evidence of poor tympanic aeration. Third, it is possible that a few patients who could not perform the Valsalva maneuver shortly after TM (up to 2 months in this study) might have been able to perform the Valsalva maneuver later, even without BDET. Therefore, a randomized study with a larger study population is necessary to elucidate the advantages of BDET. Since few studies have focused on the results of BDET in COM patients with persistent ET dysfunction, this study suggests the possibility of using BDET to treat ET dysfunction in COM patients with persistent ET dysfunction.
In summary, the Valsalva maneuver could be performed successfully after BDET in COM patients who underwent TM but still had ET dysfunction. After BDET, the air-bone gap significantly decreased, especially in patients who were capable of performing the Valsalva maneuver. Those patients could maintain an intact tympanic membrane. Therefore, BDET can be a good treatment for COM patients with persistent ET dysfunction after TM who cannot perform the Valsalva maneuver.
▪ Twenty-one ears with Eustachian tube (ET) dysfunction were examined to assess changes in patients’ ability to perform the Valsalva maneuver and audiologic improvements.
▪ None of the patients could perform a Valsalva maneuver before balloon dilation of the Eustachian tube (BDET), whereas 62% were able to perform a Valsalva maneuver after BDET.
▪ Successful performance of the Valsalva maneuver after BDET was associated with more frequent hearing improvement and intact tympanic membrane than in patients who could not perform the Valsalva maneuver successfully.
▪ BDET can be a good treatment option for chronic otitis media patients with persistent ET dysfunction.
ACKNOWLEDGMENTSThis work was supported by a Korea Medical Device Development Fund grant funded by the Korean government (the Ministry of Science and ICT, the Ministry of Trade, Industry and Energy, the Ministry of Health & Welfare, the Ministry of Food and Drug Safety) (Project Number: 1711138568, KMDF_PR_20200901_0258-01).
NotesAUTHOR CONTRIBUTIONS Conceptualization: YC, WSK, HJP. Data curation: YC, WSK. Formal analysis: YC, WSK. Funding acquisition: HJP. Investigation: HJP. Methodology: SCH, SHL. Project administration: JHA, JWC. Resources: JHA, JWC. Software: YC, WSK. Supervision: HJP. Validation: JHA, JWC. Visualization: SCH, SHL. Writing–original draft: YC, WSK. Writing–review & editing: HJP. Fig. 1.Technique of endoscopy- and fluoroscopy-guided E-tube balloon dilation. (A) Balloon was positioned in Eustachian tube orifice via endoscopy guide. (B) Guide wide was positioned in Eustachian tube via fluoroscopy guide. (C) Balloon positioned in Eustachian tube was inflated via fluoroscopy guide. 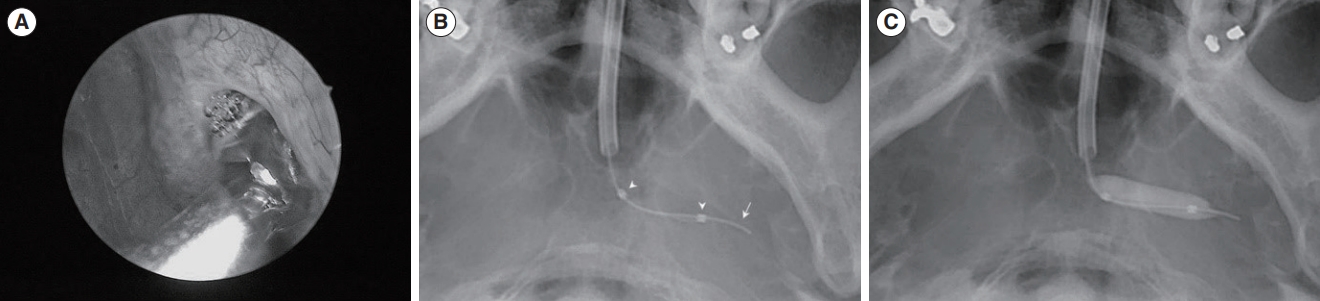
Fig. 2.Air-bone gap before and 1 year after balloon dilation of the Eustachian tube (BDET) in the successful Valsalva group (A) and the unsuccessful Valsalva group (B). VT, ventilation tube. 
Fig. 3.Changes in the air-bone gap (ABG) before and 1 year after balloon dilation of the Eustachian tube. The ABG improved by 8.9±12.4 dB in the successful Valsalva maneuver group, whereas the ABG was aggravated by 3.8±11.8 dB in the unsuccessful Valsalva maneuver group. *Statistically significant. 
Table 1.Characteristics of the patients with COM and ET dysfunction after tympanomastoidectomy Table 2.Status of the tympanic membrane in the successful and unsuccessful Valsalva groups after BDET REFERENCES1. Fliss DM, Shoham I, Leiberman A, Dagan R. Chronic suppurative otitis media without cholesteatoma in children in southern Israel: incidence and risk factors. Pediatr Infect Dis J. 1991 Dec;10(12):895-9.
2. Kim CS, Jung HW, Yoo KY. Prevalence and risk factors of chronic otitis media in Korea: results of a nation-wide survey. Acta Otolaryngol. 1993 May;113(3):369-75.
3. Stell PM. Scott-Brown’s otolaryngology. Vol. 3: management of chronic suppurative otitis media. 5th ed. Oxford: Butterworth International; 1987. p. 215-37.
4. Flint PW. Otolaryngology: head and neck surgery. Vol. 2: chronic otitis media, mastoiditis and petrositis. 6th ed. Philadelphia (PA): Saunders Elsevier; 1993. p. 2139-55.
5. Schilder AG, Bhutta MF, Butler CC, Holy C, Levine LH, Kvaerner KJ, et al. Eustachian tube dysfunction: consensus statement on definition, types, clinical presentation and diagnosis. Clin Otolaryngol. 2015 Oct;40(5):407-11.
6. Seibert JW, Danner CJ. Eustachian tube function and the middle ear. Otolaryngol Clin North Am. 2006 Dec;39(6):1221-35.
7. Adil E, Poe D. What is the full range of medical and surgical treatments available for patients with Eustachian tube dysfunction. Curr Opin Otolaryngol Head Neck Surg. 2014 Feb;22(1):8-15.
8. Llewellyn A, Norman G, Harden M, Coatesworth A, Kimberling D, Schilder A, et al. Interventions for adult Eustachian tube dysfunction: a systematic review. Health Technol Assess. 2014 Jul;18(46):1-180.
9. Ockermann T, Reineke U, Upile T, Ebmeyer J, Sudhoff HH. Balloon dilatation eustachian tuboplasty: a clinical study. Laryngoscope. 2010 Jul;120(7):1411-6.
10. Poe DS, Metson RB, Kujawski O. Laser eustachian tuboplasty: a preliminary report. Laryngoscope. 2003 Apr;113(4):583-91.
11. Metson R, Pletcher SD, Poe DS. Microdebrider eustachian tuboplasty: a preliminary report. Otolaryngol Head Neck Surg. 2007 Mar;136(3):422-7.
12. Smith ME, Tysome JR. Tests of Eustachian tube function: a review. Clin Otolaryngol. 2015 Aug;40(4):300-11.
13. Poe DS, Silvola J, Pyykko I. Balloon dilation of the cartilaginous Eustachian tube. Otolaryngol Head Neck Surg. 2011 Apr;144(4):563-9.
14. Huisman JM, Verdam FJ, Stegeman I, de Ru JA. Treatment of Eustachian tube dysfunction with balloon dilation: a systematic review. Laryngoscope. 2018 Jan;128(1):237-47.
15. Kim Y, Kang WS, Kang JM, Ryu DS, Kwak MY, Song HY, et al. Technical feasibility and histological analysis of balloon-expandable metallic stent placement in a porcine Eustachian tube. Appl Sci. 2021 Jan;11(4):1359.
16. Park JH, Kang WS, Kim KY, Kang BC, Park JW, Kim MT, et al. Transnasal placement of a balloon-expandable metallic stent: human cadaver study of the Eustachian tube. J Vasc Interv Radiol. 2018 Aug;29(8):1187-93.
17. Kim KY, Kang WS, Park JH, Kang BC, Park JW, Kim MT, et al. Fluoroscopic subtraction eustachian tubography: initial feasibility test in a cadaver model. Eur Radiol. 2018 Sep;28(9):3685-91.
18. Poe DS, Hanna BM. Balloon dilation of the cartilaginous portion of the Eustachian tube: initial safety and feasibility analysis in a cadaver model. Am J Otolaryngol. 2011 Mar-Apr;32(2):115-23.
19. Ockermann T, Reineke U, Upile T, Ebmeyer J, Sudhoff HH. Balloon dilation eustachian tuboplasty: a feasibility study. Otol Neurotol. 2010 Sep;31(7):1100-3.
20. McCoul ED, Singh A, Anand VK, Tabaee A. Balloon dilation of the eustachian tube in a cadaver model: technical considerations, learning curve, and potential barriers. Laryngoscope. 2012 Apr;122(4):718-23.
21. Catalano PJ, Jonnalagadda S, Yu VM. Balloon catheter dilatation of Eustachian tube: a preliminary study. Otol Neurotol. 2012 Dec;33(9):1549-52.
22. McCoul ED, Anand VK. Eustachian tube balloon dilation surgery. Int Forum Allergy Rhinol. 2012 May-Jun;2(3):191-8.
23. Silvola J, Kivekas I, Poe DS. Balloon dilation of the cartilaginous portion of the Eustachian tube. Otolaryngol Head Neck Surg. 2014 Jul;151(1):125-30.
24. Wanscher JH, Svane-Knudsen V. Promising results after balloon dilatation of the Eustachian tube for obstructive dysfunction. Dan Med J. 2014 Apr;61(4):A4818.
25. Bowles PF, Agrawal S, Salam MA. Balloon tuboplasty in patients with Eustachian tube dysfunction: a prospective study in 39 patients (55 ears). Clin Otolaryngol. 2017 Oct;42(5):1057-60.
26. Poe D, Anand V, Dean M, Roberts WH, Stolovitzky JP, Hoffmann K, et al. Balloon dilation of the eustachian tube for dilatory dysfunction: a randomized controlled trial. Laryngoscope. 2018 May;128(5):1200-6.
27. Demir B, Batman C. Efficacy of balloon Eustachian tuboplasty as a first line treatment for otitis media with effusion in children. J Laryngol Otol. 2020 Nov;134(11):1018-21.
28. Toivonen J, Kawai K, Gurberg J, Poe D. Balloon dilation for obstructive Eustachian tube dysfunction in children. Otol Neurotol. 2021 Apr;42(4):566-72.
29. Kim KY, Tsauo J, Song HY, Park HJ, Kang WS, Park JH, et al. Fluoroscopy-guided balloon dilation in patients with Eustachian tube dysfunction. Eur Radiol. 2018 Mar;28(3):910-19.
30. Song HY, Park HJ, Kang WS, Kim KY, Park JH, Yoon SH, et al. Fluoroscopic balloon dilation using a flexible guide wire to treat obstructive Eustachian tube dysfunction. J Vasc Interv Radiol. 2019 Oct;30(10):1562-6.
31. Kang BC, Kang WS, Park JW, Park JH, Kim KY, Song HY, et al. Fluoroscopic balloon diameter measurement at different pressures during Eustachian balloon dilation. Clin Otolaryngol. 2018 Dec;43(6):1573-7.
32. Xiong H, Liang M, Zhang Z, Xu Y, Ou Y, Chen S, et al. Efficacy of balloon dilation in the treatment of symptomatic Eustachian tube dysfunction: one year follow-up study. Am J Otolaryngol. 2016 Mar-Apr;37(2):99-102.
|
|
|||||||||||||||||||||||||||||||||||||||||







