INTRODUCTION
Maxillofacial trauma has recently increased due to increases in social activities and advances in diagnostic methods (1). The evaluation and treatment of maxillofacial trauma tends to be delayed when it is associated with injuries to other parts of the body. If treatment is delayed due to concurrent systemic diseases, permanent facial deformities may be unavoidable because surgical manipulation is frequently difficult or even impossible. Considering that maxillofacial injuries occur mostly in younger subjects (2), the problem of aesthetic outcome is especially serious.
We report herein the case of a young adult in whom facial deformity occurred because the fractured bones were fused after a delay in early management due to his severe hyperthyroidism. He was satisfactorily treated by surgery. A brief review of the literature has been included.
CASE REPORT
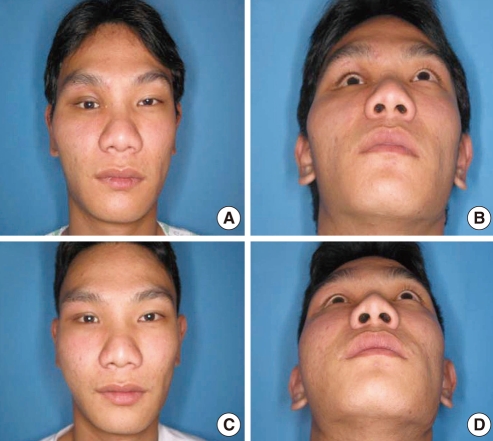
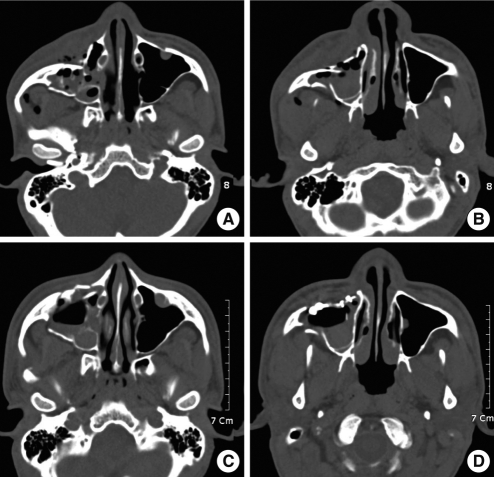
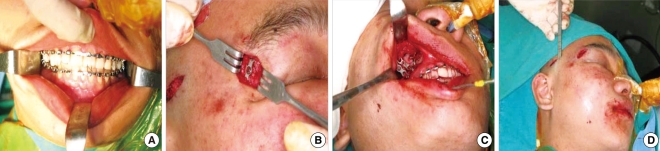
A 21-yr-old man presented at our department with the chief complaint of right facial edema and deformity that occurred after a blow to the facial area. Physical examination showed loss and asymmetry of the right zygomatic eminence, depression of the right eyeball and difficulty in mouth opening (Fig. 1A, 1B). Facial bone computed tomography (CT) revealed a right tetrapod fracture with posterior displacement due to fractures of the anterior and posterior walls of the right maxilla and the right zygoma (Fig. 2A, 2B). A fracture of the orbital inferior wall was also noted. Neither restriction of eyeball movement nor visual disturbance was observed. We decided to perform open reduction of the right tetrapod fracture and the right orbital inferior wall fracture. However, thyroid function tests exhibited increases in levels of T3, T4 and free T4 and a decrease in the TSH level due to concurrent underlying hyperthyroidism. The patient underwent medical treatment for hyperthyroidism at the Department of Internal Medicine for 2 months and was then transferred to our department for surgery. We decided to perform surgical treatment because the patient's facial deformity was severe. We performed intermaxillary fixation to prevent malocclusion during fixation (Fig. 3A). We confirmed the extent of the fracture and fusion through both a lateral eyebrow incision and a gingival isthmus incision (Fig. 3B, 3C). The fractured sites were displaced and fused. We obtained sufficient mobility by refracturing the zygomaticomaxillary fusion site and zygomaticofrontal fusion site with a 2-mm osteotome. We attempted to refracture the zygomatic arch fusion site through a gingivobuccal incision, but a temporal incision was made because of the limited surgical field. We obtained sufficient mobility by fracturing the zygomatic arch with a 4-mm osteotome (Fig. 3D). The displaced bone was reduced to its normal anatomical location. The zygomaticofrontal and zygomaticomaxillary areas were fixed with miniplates and screws. An ophthalmologist corrected eyeball depression caused by the orbital inferior wall fracture by inserting a medpor through a transconjunctival incision. After surgery, facial appearance and difficulty in mouth opening improved (Fig. 1C, 1D).
On the three-dimensional facial bone CT scans, the displaced bone was reduced to its normal anatomical location (Fig. 2C, 2D). At 6-month follow-up, the patient complained of no particular discomfort in everyday life activities and was satisfied with his external appearance.
DISCUSSION
Traumas to the head and neck area can result from various causes including traffic accidents, violence, sports injuries and industrial accidents. It has been reported that associated injuries occur in approximately 30 percent of patients who sustain facial trauma (3). Maxillofacial injuries are often neglected in patients with serious clinical conditions such as intracranial injury and injury to the cervical spine. In cases that have neurosurgical conditions or underlying medical diseases, surgical manipulation may be difficult, and the success rate of the surgery may be lowered due to the delay in treatment. Fracture sites start to heal spontaneously 10 to 14 days after trauma without immediate management. It is generally accepted that fracture reduction is difficult or impossible in delayed cases even with the maximal force possible with an extractor. Such delayed cases may require surgical procedures such as loosening of the bony fragment by refracturing previous fracture sites with an osteotome (4) or plugging up the defect area using grafts (5). In our case, the initial management was delayed because of hyperthyroidism. We had great difficulty in performing reduction because of malalignment of the fracture line. Therefore, we refractured the fracture line with an osteotome in order to obtain sufficient mobility and fixed it using miniplates and screws.
Tetrapod fracture may result in severe facial deformity and involve the orbit and maxillary sinus. To prevent aesthetic and functional sequelae, tight accurate fixation is essential (6). In particular, the zygomatic bone is an anatomical structure that determines the outer shape of the mid face. If zygomatic fracture is associated with orbital wall fracture, it must first be corrected according to the guidelines for orbital wall fracture correction (7, 8). In our case, we made a temporal incision in order to obtain the wide surgical visual field for refracturing the fused zygomatic arch. This procedure seemed to be a good approach. Ophthalmologists usually perform infraorbital wall fracture reduction through a transconjunctival incision. However, this conventional transorbital approach has many problems such as extrusion or absorption of implanted materials and infection or scar formation after surgery. Therefore, the nasal-endoscopic endonasal reduction technique (9) is thought to be a better surgical procedure. This technique has several advantages: because it is conducted without a skin incision, it has a better aesthetical outcome; there is less bleeding; and it enables surgeons to confirm that the reduction is exact during surgery.
The facial area is important in aesthetic and functional aspects. Thus, accurate diagnosis and early treatment are of crucial importance. Good cosmetic outcome is achievable in maxillofacial trauma patients, even in those with associated injuries and concurrent systemic diseases. Early evaluation and timely intervention can avoid unnecessary treatments and prevent postoperative complications. Furthermore, we consider refracturing of the fusion site with an osteotome to be a good procedure for obtaining sufficient motility and accurate fixation.