INTRODUCTION
Idiopathic sudden sensorineural hearing loss (SSNHL) is defined as a decline in hearing over 3 days or less and this affects three or more frequencies by 30 dB or greater without an identifiable etiology, and it may vary from mild to profound hearing impairment. Steroids appear to be the only efficacious treatment in controlled clinical trials (1). Systemic steroids produce significant hearing improvement for patients with moderate to severe SSNHL (2), while the patients with profound SSNHL have a poor prognosis regardless of the treatment (3, 4).
Intratympanic dexamethasone (ITD) produces significantly higher perilymph concentrations of steroids than does intravenous or oral administration (5, 6). Although its efficacy has not been proven, intratympanic steroids are being increasingly used as a therapeutic option for SSNHL worldwide. The published data shows that intratympanic steroids in SSNHL are mostly used as salvage treatment after systemic steroids (7). However, the efficacy of ITD for severe to profound SSNHL has not yet been determined.
This study evaluated the effect of using ITD as a salvage treatment for severe to profound SSNHL.
MATERIALS AND METHODS
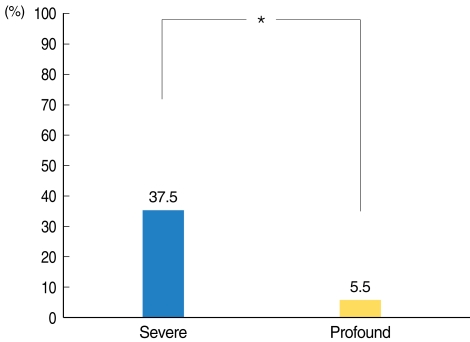
We reviewed the medical records of all patients with SSNHL and who were seen from January 2007 and December 2009 at our hospital. This study was approved by the Institutional Review Board of the Soonchunhyang University College of Medicine. The patients with unilateral SSNHL with an average hearing loss greater than 70 dB across four frequencies (500, 1,000, 2,000, and 3,000 Hz), were included in this study. The patients were divided into two groups: the severe hearing loss group with a loss between 70 and 90 dB (25 patients) and the profound hearing loss group with a loss greater than 90 dB (22 patients).
All the patients were hospitalized and they were all were treated with intravenous dexamethasone (10 mg/d for 5 days, 7.5 mg/d for 2 days) for seven days and then with oral steroids (prednisolone) for 3 days in tapered doses after the patients were discharged from the hospital. We performed audiometry 2 weeks after the primary systemic steroid treatment. If the patient did not show a complete or partial recovery, then we considered them for ITD as salvage treatment. The intratympanic steroid injection was repeated for a total of six injections over 2 weeks. Topical anesthesia was applied with 10% lidocaine spray from a spray pump. With the patient in the supine position and with the head tilted 45° to the opposite side, a 25-gauge spinal needle was passed through the anterosuperior portion of the tympanic membrane. Approximately 0.3 to 0.4 mL of dexamethasone (5 mg/mL) was instilled.
Successful recovery at 1 month after ITD therapy was defined as complete or partial recovery using Siegel's criteria. "complete recovery" was defined as final hearing better than 25 dB and "partial recovery" as a hearing gain exceeding 15 dB and the final hearing was between 25 and 45 dB.
Statistical tests were performed using Fischer's exact test for categorical variables and Student's t-test for continuous variables (SPSS ver. 14.0, SPSS Inc., Chicago, IL, USA).
RESULTS
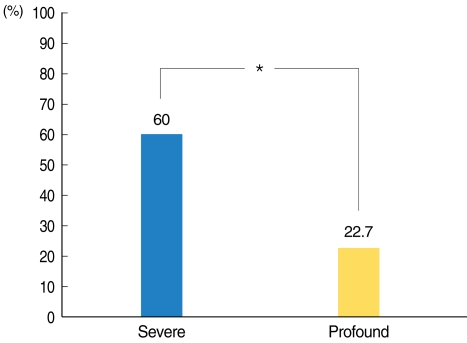
The demographics and audiological data of the patients are summarized in Table 1. The patients in the severe SSNHL group showed significant overall improvement compared with that of the profound SSNHL group (Fig. 1).
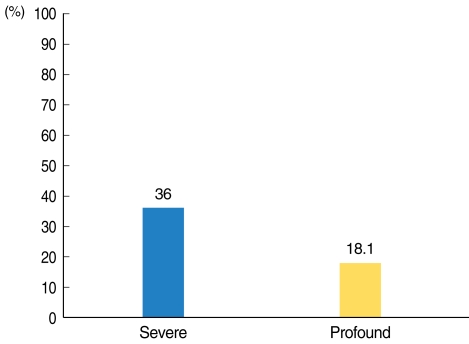
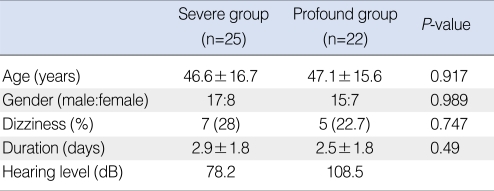
The early recovery rate 2 weeks after the initial systemic treatment was 36% (9/25) in the severe SSNHL group and 18.1% (4/22) in the profound SSNHL group (Fig. 2). By contrast, the recovery rate of ITD as a salvage treatment was 37.5% (6/16) in the severe SSNHL group and 5.5% (1/18) in the profound SSNHL group (Fig. 3). The total recovery rate of ITD as a salvage treatment for the patients with severe to profound SSNHL was 20.6% (7/34).
Of the patients in the severe SSNHL group who recovered after ITD, four showed complete recovery and two patients showed partial recovery. The only patient who recovered after ITD in the profound SSNHL group showed partial recovery.
DISCUSSION
This study examined the efficacy of ITD as a salvage treatment for severe to profound SSNHL. SSNHL is a very frightening and incapacitating event and it severely impairs the patient's quality of life and ability to interact socially. Patients with severe to profound SSNHL have difficulty with hearing rehabilitation such as hearing aids if their hearing recovery is poor.
The use of intratympanic steroids (ITS) has evolved into three main protocols for the treatment of SSNHL. In the first, ITS are used as adjuvant treatment and they are given concomitantly with systemic steroids for SSNHL. Battaglia et al. (8) reported that combination therapy (ITD+systemic steroid) had a greater likelihood of inducing hearing recovery than systemic steroid alone. Ahn et al. (9) reported that the addition of ITD to systemic steroids did not result in a significant improvement in the treatment of SSNHL; however, these findings are in contrast to the results of Battaglia et al. (8). We did not choose this modality for treating SSNHL because even the patients who show good recovery with systemic steroid alone would be given unnecessary ITD.
In the second modality, ITS are used as the initial or primary treatment for SSNHL without systemic steroid. The primary reason is to avoid systemic side effects, such as peptic ulcers and osteonecrosis. Kara et al. (10) reported that ITD alone achieved better hearing results than systemic steroids, while Hong et al. (11) reported that the group given ITD as primary therapy showed no difference in the hearing recovery, as compared with the systemic steroid group, although the threshold of the improvement was greater in the systemic steroid group than in the ITD group at high frequencies (4 and 8 kHz). However, only two papers have studied the effect of intratympanic steroids as primary therapy without systemic steroids. More studies are needed to clarify the effect of this modality. In addition, the side effects of systemic steroids in patients with SSNHL are very rare because side effects are usually associated with long-term therapy and ITD has potential negative outcomes such as pain, tympanic membrane perforation, otorrhea and vertigo. On the other hand, this modality has an advantage for patients with diabetes because systemic steroids in patients with diabetes require paying very close attention to the glycemic control. Han et al. (12) reported that ITD is as effective as systemic steroid treatment for SSNHL patients with diabetes.
In the third modality, ITS are used as salvage therapy after the failure of systemic steroids for SSNHL. The majority of studies in the literature concerning the use of ITS in the treatment of SSNHL has reported on this as salvage therapy. The percentage of successful treatment after ITD has ranged from 12% to 100% because each study used different criteria to assess improvement (10, 13). Many authors defined successful treatment as a 10 or 15 dB improvement. A few studies defined it as a 20 or 30 dB improvement on PTA (13, 14). In comparison, we defined "successful recovery" as complete and partial recovery using Sigel's criteria, with excluding slight recovery. If we included mild improvement, such as a 10 or 15 dB gain, in successful recovery, then the recovery rate would be higher. For cases of severe to profound hearing loss, we believed that a mild improvement would not satisfy the patients.
Our treatment protocol consists of systemic steroids and then ITD as salvage treatment. First, we performed audiometry 2 weeks after the primary systemic steroid treatment. If the patient did not show a complete or partial recovery, then we considered them for ITD as salvage treatment. When to start the salvage treatment is controversial. Moon et al. (15) reported that the prognosis of SSNHL could be predicted approximately 2 weeks after the start of treatment because the time of commencement shows a plateau after 2 weeks in the cases that improved.
We showed that the efficacy of ITD significantly differed between the severe and profound SSNHL groups. It has been previously demonstrated that systemic steroids in patients with profound SSNHL result in an extremely poor prognosis. Our study showed that ITD as salvage treatment for patients with profound SSNHL also has a very poor prognosis.
Our comparative study does not support the efficacy of ITD as a salvage treatment for patients with profound SSNHL as compared with that for severe SSNHL. We recommend that patients with profound SSNHL be informed of the low efficacy of ITD as a salvage treatment.