Classification of External Auditory Canal Cholesteatoma by Computed Tomography
Article information
Abstract
Objectives
We propose here a classification system for external auditory canal cholesteatoma (EACC). We classified the EACC by the computed tomography findings and clinical findings of the patients, and we evaluated the EACC characteristics by the proposed staging system.
Methods
Stage classification was done according to the results of temporal bone computed tomography and the clinical findings of the patients. Stage I indicates that the EACC lesion is limited to the external auditory canal. Stage II indicates that the EACC lesion invades the tympanic membrane and middle ear. Stage III indicates that the EACC lesion creates a defect of the external auditory canal and it involves the air cells in the mastoid bone. Stage IV indicates that the EACC lesion is beyond the temporal bone. Between 1996 and 2006, 29 patients with EACC and who underwent surgery were prospectively collected. This study was comprised of 16 males and 13 females with a mean age of 22.8±15.0 yr. We reviewed the characteristics and results of surgery by our proposed staging system.
Results
A total of 29 patients who underwent operation due to EACC were classified by this system, and the number of stage I, II, III, and IV cases was 14, 3, 10, and 2, respectively. Symptoms such as otorrhea, hearing impairment and otalgia occurred in 12, 17, and 17 cases, respectively. The most common wall invaded by EACC was the inferior wall. The number of cases that had a spontaneous, congenital, post-traumatic, post-inflammatory or tumorous origin was 14, 9, 2, 2, and 1, respectively. Cholesteatoma recurred in 2 patients after surgery. Both cases were stage 1 and both were caused by congenital disease. There were 3 cases with meatal stenosis after surgery, and their primary disease was congenital.
Conclusion
This proposed staging is simple and easily applicable for use when deciding the treatment plan for patients with EACC.
INTRODUCTION
A cholesteatoma is a bone-destructive cystic mass that is lined by stratified keratinizing squamous epithelium, and this cystic mass is in an abnormal location such as the middle ear, the petrous apex or the external auditory canal. It is mostly found in the middle ear and rarely in the external auditory canal (1). External auditory canal cholesteatoma (EACC) was first described in 1850 by Toynbee (2). Since then, it had been confused with keratosis obturans, and it was distinguished by Piepergerdes et al. (3) in 1980. They showed that keratosis obturans results from the accumulation of large plugs of desquamated keratin in the ear canal, and EACC is due to an invasion of squamous tissue into a localized area of periosteitis in the canal wall. The etiology and pathophysiology of cholesteatoma have not yet been established.
The classification of the EACC stage by the histology and clinical symptoms of the patients was first reported by Naim et al. (4) in 2005. This system can express the exact range of EACC lesions after surgery.
It is known that the cause of congenital EACC is stenosis of the EAC and that of spontaneous EACC is uncertain (5).
We wanted to introduce a staging system that gives surgeons the information they need to decide the proper treatment and surgery before an operation. The aim of this study was to propose a staging system for EACC, to classify EACC according to the computed tomography findings and the clinical findings of patients, and to evaluate the characteristics of EACCs by this method.
MATERIALS AND METHODS
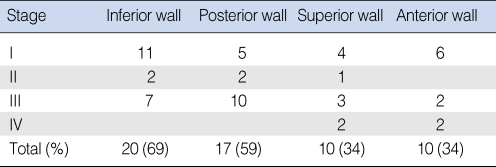
Stage classification was done according to the results of temporal bone computed tomography and the clinical findings of the patients. We defined the EACC stages as follows: stage I indicates that the EACC lesion is limited to the external auditory canal, stage II means that the EACC lesion invades the tympanic membrane and middle ear, stage III is when the EACC lesion creates a defect of the external auditory canal and involves the air cells in the mastoid bone, and stage IV indicates that the EACC lesion is beyond the temporal bone. (Table 1, Fig. 1).

Definition for the proposed stagings of external auditory canal cholesteatoma and the number of cases by the stage (N=29)
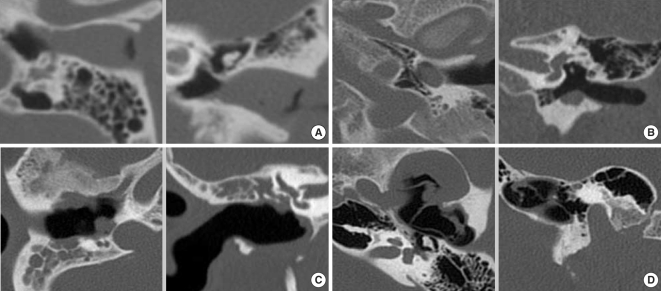
4 stages of external auditory canal cholesteatoma (EACC) on temporal bone computed tomography. (A) Stage I. The lesion was within the external auditory canal. (B) Stage II. The lesion invaded the middle ear. (C) Stage III. The lesion invaded the mastoid cavity. (D) Stage IV. The lesion extended beyond the temporal bone.
Between 1996 and 2006, 29 patients with EACC and who underwent surgery at our institute and who could be followed up more than 6 months were prospectively collected. The study was comprised of 16 males and 13 females with a mean age of 22.8±15.0 yr. We analyzed the characteristics of the EACC and the results of surgery by our proposed staging system.
The treatment strategy was as follows: stage I required only canaloplasty, stage II required canaloplasty and tympanoplasty, stage III required canaloplasty and mastoidectomy, and if the middle ear was invaded, it also required tympanoplasty, and stage IV required that surgery should be tailored according to the site of the lesion (Table 1).
If there was no apparent cause for an EACC in the patients who did not have a narrow external auditory canal, then it was classified into spontaneous EACC. If the patient had a narrow external auditory canal, then it was classified into congenial EACC.
RESULTS
A total of 29 patients who underwent surgery due to EACC were classified by this method, and the number of stage I, II, III, and IV cases was 14, 3, 10, and 2, respectively (Table 1). Otorrhea, hearing impairment and otalgia occurred in 12, 17, and 17 patients, respectively. The most common wall invaded by EACC was the inferior wall (Table 2). The primary causes of EACC are spontaneous, congenital, post-traumatic, post-inflammatory EACC and tumor, and the number of EACCs in our study with these causes was 14, 9, 2, 2, and 1, respectively. Table 2 shows the distribution of the walls involved by EACC in terms of this staging.
There were 2 cases of stage IV EACC. One case was an EACC from the external auditory canal that extended into the temporomandibular joint through the anterior wall of the external auditory canal and this was managed by the transcanal approach. The other case was that an EACC from the external auditory canal extended superiorly into the middle cranial fossa and this was treated by the middle cranial fossa approach and the transcanal approach.
There were 2 cases in which cholesteatoma recurred after surgery. The stage and the primary disease in both these patients were stage I and congenital disease, respectively. The reason for recurrence may be that the hidden cholesteatoma epithelium debris was not fully removed at surgery. Both patients underwent revision surgery.
There were 3 cases of meatal stenosis after surgery, with one case in stage I and two cases in stage III, and the primary cause of all 3 cases was congenital. The case in stage I underwent revision surgery and the postoperative stenosis of the other 2 stage III cases was managed with inserting a nelaton catheter into the external auditory canal.
DISCUSSION
It is known that except for the case of a very limited lesion, the principle of treatment for EACC is preservation of the normal external auditory canal skin and surgical removal of the cholesteatoma and necrotic bone tissue to prevent disease progression and bone destruction. The precise limit of surgical removal is determined by the degree of bone necrosis and bony erosion and the surgeon's judgment. Surgeons should consider whether the middle ear, mastoid cavity, facial nerve, labyrinth and ossicles are involved so that in the case that the lesion is limited to the external auditory canal, it can be treated by only local care (6) or canaloplasty, as defined by stage I. In the case that the lesion invades the middle ear in addition to the external auditory canal, it can be managed by canaloplasty and tympanoplasty as defined by stage II. When the lesion invades the mastoid air cells as defined by stage III, the patient can be managed with canaloplasty, mastoidectomy and optional tympanoplasty. In the stage III cases, reconstruction of the EAC wall can be performed with bone dust. In the case that the lesion progresses beyond the temporal bone as defined by stage IV (e.g., the glenoid fossa or middle fossa), the cholesteatoma can be removed via various approaches such as the middle fossa approach or the transzygomatic approach.
Our staging system does not require the postoperative pathologic results, which is in contrast to the classification systems by other authors (4), and it can be applied to preoperative evaluation.
According to our data, there were few cases of stage II and IV. For stage II, the epicenter of the cholesteatoma is within the external auditory canal and it can easily involve the air cells of the mastoid cavity, and there are many cases in which the lesion is apart from the middle ear cavity. In our study, the EACC mostly invaded the inferior wall. All the stage III cases involved the posterior wall of the external auditory canal.
The surgical results were as follows: cholesteatoma recurred after surgery in 2 stage 1 cases of a congenital origin and meatal stenosis occurred in 3 cases. The origin of the meatal stenosis was also congenital. This may indicate that there are more postoperative complications in the congenital EACC cases than in the other types of cases. This proposed staging is simple and easily applicable for use when deciding the treatment plan.
Notes
No potential conflict of interest relevant to this article was reported.