Functional Benefit after Modification of Radial Forearm Free Flap for Soft Palate Reconstruction
Article information
Abstract
Objectives
To compare the velopharyngeal function, swallowing and speech of the conventional and modified radial forearm free flap (RFFF) for soft palate reconstruction.
Methods
Retrospective clinical study. Twenty-eight patients who underwent oropharyngeal reconstruction with RFFF were divided into two groups: 10 patients had conventional folded RFFF and 18 patients underwent modified method.
Results
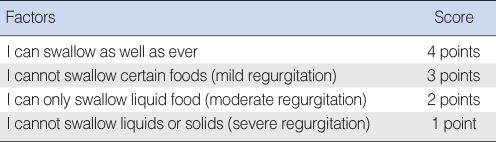
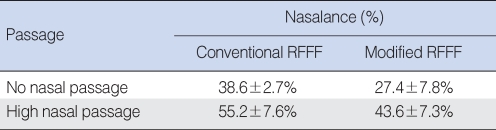
The average speech intelligibility score in modified RFFF group was 8.0±2.4, and 6.2±2.2 in conventional RFFF group (P<0.05). The nasalance was 27.4±7.8% in modified group and 38.6±2.7% in conventional group during no nasal passage reading and 43.6±7.3% in modified group, 55.2±7.6% in conventional group during high nasal passage reading (P<0.05). The subjective swallowing functional score was 2.8 in modified group and 2.1 in conventional group.
Conclusion
The speech assessment and nasalance demonstrate a more favorable outcome in modified group than conventional group.
INTRODUCTION
The defects of the soft palate are difficult to reconstruct because of their complicated anatomy and causing velopharyngeal incompetence for speech and swallowing function. Many reconstruction techniques have been described to improve postoperative function after oropharyngeal resection including soft palate, but the use of these heterogeneous procedures has resulted in variable speech and swallowing outcome. Recently, reconstructive options have been significantly expanded and revitalized by the advent of free tissue transfer. The thin, pliable nature of the fasciocutaneous flaps is ideally suited for oropharyngeal reconstructions, especially when the defect involves multiple sites, such as the pharyngeal wall, soft palate, and tongue base. The radial forearm free flaps (RFFF) have been widely used for soft palate reconstruction, but the reconstructed soft palate contracts during the healing phase and there is a risk of an increasing space developing between the reconstructed soft palate and posterior pharyngeal wall (1). This effect is likely to be increased during postoperative radiotherapy as a result of further shrinkage and poor mobility due to fibrosis (2). We have modified the conventional RFFF by de-epithelialization of medial margin of the flap for reconstruction of the soft palate to minimize postoperative velopharyngeal incompetence.
The purpose of this study is to introduce our modification method of radial forearm free flap and to compare the velopharyngeal function, swallowing and speech, of the conventional and modified radial forearm free flap for soft palate reconstruction.
MATERIALS AND METHODS
Patient characteristics
From January 1995 to December 2001, 28 patients who underwent soft palate and lateral oropharyngeal reconstruction with a RFFF in surgical management of tonsil cancer were evaluated for postoperative speech and swallowing function in present stud y. The size of the soft palate resection was estimated by examining the patient at the time of assessment. Minimal soft palate resections were graded one quarter. Larger resections were graded one half if the uvula was not included and three quarter if it was part of the resection. Patients were eligible for this study if the posterior margin of the soft palate was included in the resection and the soft palate defects extended one half to three quarter. All patients of two groups had intact contralateral lateral oropharyngeal-including palatopharyngeal, palatoglossal, and superior constrictor-muscles matched by size of the soft palate resection. Of this group in 28 patients, 10 patients underwent reconstruction by conventional RFFF and 18 patients underwent reconstruction by modified RFFF. Patients received a standard protocol of postoperative radiotherapy at one institution when needed. No patients received speech therapy during the time of follow-up, but all patients had swallowing therapy before discharge from the hospital.
Resection and reconstruction
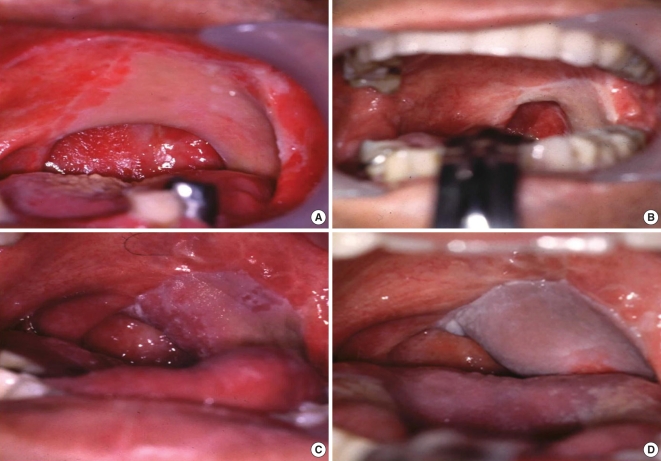
For the resection of the soft palate, the access preferred was a mandibulotomy approach and delivery of the en bloc resection in continuity with neck dissection. Once the resection was completed, the size and shape of the defect was mapped onto a piece of sterilized paper, and used by the team raising the flap on the forearm. The conventional RFFF was designed with bi-lobed or tri-lobed on distal part of the flap and sutured to the mucosal edge of anterior soft palate, posterior oropharyngeal wall, and lateral tongue or mucosa of retromolar trigone (Fig. 1). In the modified RFFF, the medial margin of the flap was sutured to the mucosal edge of the posterior oropharyngeal wall toward the nasopharynx, and the area of the flap in contact with the cut end of the soft palate is de-epithelialized and sutured to the remaining soft palate (Fig. 2, 3).
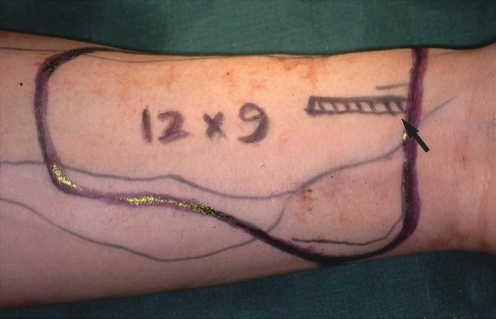
Design for modified radial forearm free flap. Tri-lobed flap of which some portion was de-epithelialized (arrow) and sutured to the remaining soft palate.
Postoperative functional assessment
At least 6 months after surgery, speech and swallowing function was evaluated. Speech intelligibility was evaluated with the 10-point scoring system of Hirose (3) and the presence of hypernasality was assessed (Table 1). And for objective assessment, we measured nasalance with nasometer (Model 6200B, KAY Elemetrics Corp., Lincoln Park, NJ, USA), which reflects the ratio of acoustic energy output of nasal sounds from the nasal and oral cavity. The nasalance (%) was measured during the patient read the no nasal passage (nasal consonant ratio [NCR] 0%) and high nasal passage (NCR 34.7%). Swallowing function was evaluated by a questionnaire. The Seattle questionnaire (4) was used to assess swallowing (Table 2).
A statistical analysis using the Fisher's exact test was undertaken to compare the functional outcome between conventional RFFF and modified RFFF.
RESULTS
Patient data
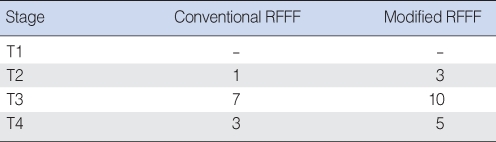
From January 1995 to December 2001, 28 patients who had soft palate and lateral oropharyngeal wall excised because of squamous cell carcinomas of the tonsil subsequently underwent primary reconstruction with RFFF. They had received no prior radiotherapy and chemotherapy before surgical treatment. The 28 patients (20 male and 8 female) ranged in age from 36 to 77 yr (average age, 62.4 yr). Ten patients underwent reconstruction by conventional RFFF and 18 patients underwent reconstruction by modified RFFF. In 10 conventional RFFF, tumors were classified as T2 in 1 patient, T3 in 7, and T4 in 3. And in 18 modified RFFF, T2 in 3, T3 in 10, and T4 in 5 patients (Table 3). Neck dissection had been performed in all patients, and postoperative radiotherapy had been performed in 26 patients. The mean follow up duration was 32 months and speech and swallowing function was evaluated at least 6 months after surgery. Each functional evaluation was performed by same speech therapist and doctor. Add on functional evaluation, they interviewed patients themselves and their family members.
Postoperative function
The average speech intelligibility score in modified RFFF group was 8.0±2.4, and 6.2±2.2 in conventional RFFF group (P<0.05). The nasalance was 27.4±7.8% in modified RFFF group and 38.6 ±2.7% in conventional RFFF group during no nasal passage reading and 43.6±7.3% in modified RFFF group, 55.2±7.6% in conventional RFFF group during high nasal passage reading (P<0.05) (Table 4). The subjective swallowing functional score by the Seattle questionnaire was 2.8 in modified RFFF group, 2.1 in conventional RFFF group.
DISCUSSION
Because of complex function and anatomy of oropharynx, reconstruction after ablation surgery for oropharyngeal cancer is always challenge to the head and neck reconstructive surgeon. Among of various reconstruction methods, free flap transfer is widely used method to reconstruct defect following head and neck cancer surgery recently. Especially RFFF is the most common flap to reconstruct oral cavity and oropharynx because skin is thin, pliable, abundant and well vascularized, which allows for considerable freedom in flap design and in accurate insetting (5). But, not only natural healing process but also adjuvant radiation therapy following head and neck ablation surgery can cause considerable loss of flap volume and constrict flap and adjunctive mucosal tissue. So a head and neck reconstructive surgeon must predict volume loss of flap after surgery and radiation therapy. To reduce flap contracture and shrinkage, we modified RFFF by de-epithelialize the cut end area of the soft palate of flap and sutured to the remaining soft palate. Kimata et al. (6) used denude method (7) that is similar to ours in flap design and surgical technique. They suggested that denude method should be used to fill more extensive defects and to narrow the velopharyngeal space. This method could easily fill defects; however, the velopharyngeal space is somewhat difficult to control.
The results of speech assessment demonstrate a more favorable speech outcome reported in modified RFFF group with an average speech intelligibility score of 8.0 compared with 6.2 in conventional RFFF group. And these findings confirmed by the results of nasalance measurement. The nasalance in modified RFFF group was significantly less than in conventional RFFF group both no nasal passage and high nasal passage. It is because the speech function is influenced by the velopharyngeal space, and narrowing the velopharyngeal space is important for obtaining satisfactory speech functional results (6). Comparing with conventional RFFF, we can get more sufficient volume with this modified RFFF, and that, it is possible to decrease the size of velopharynx by shortening the distance between the posterior pharyngeal wall and the modified RFFF flap (Fig. 3). On the other hand, there might be two possible weak points, first, this procedure may cause temporary bulkiness of initial flap, but it's not the essential problem of airway because tracheostomy was performed for all patients. Second, it's not easy to calculate precise length of remaining soft palate after resection. But assessment of swallowing does not demonstrate an obvious advantage in modified RFFF group (2.8 in modified RFFF group, 2.1 in conventional RFFF group). The reason of no statistical difference in swallowing function between modified and conventional RFFF group is that swallowing is more affected by the extent of resection rather than by the type of flap used for reconstruction (8). And our patients had more advanced-staged tonsil cancer, so that more extensive resection of soft palate had been required. We recognized the reduced swallowing function after radiation therapy due to the dysmotility of the oropharyngeal and laryngeal structures. But we did not compare the swallowing function between postoperative radiation and postoperative non-radiation group because the size of postoperative non-radiation group (n=2) is too small to compare.
The acknowledged weaknesses of the present study include, first, small sample size, which may have resulted in limited statistical power. And second, the extent of resection and volume of resection was not considered in this study. Third, patients with poorer functional outcome are more likely to drop out of a longitudinal study, which may lead to bias in the results and understatement of the level of dysfunction.
CONCLUSIONS
The surgical modification for reconstruction of soft palate and lateral oropharyngeal defect has been suggested in this study. This comparative analysis indicates the potential advantage of the modified RFFF, although further study is important to substantiate these results.
Notes
All authors had no conflict of interest on this study.