Venous Hemangioma of Parapharyngeal Space with Calcification
Article information
Abstract
A hemangioma of the parapharyngeal space (PPS) is an extremely rare tumor and is responsible for 0.5-1% of all tumors occurring in the PPS. We report a case of PPS venous hemangioma in a 49-year-old woman presenting with diffuse swelling in the submandibular region. A preoperative computed tomography (CT) scan showed a cystic mass with multiple calcifications in the PPS. The calcific nodules were round and about 2 mm in diameter. The hemangioma was completely resected via a transcervical approach. During surgery, we found several calcific nodules, which represented phleoboliths or areas of thrombosis with dystrophic calcification. Despite its rarity, a venous hemangioma of the PPS should be considered in a differential diagnosis when a cystic mass with calcification is found by CT scan. To our knowledge, this is the first reported case of a PPS venous hemangioma; we describe its pathognomonic findings on imaging.
INTRODUCTION
Hemangiomas are categorized as racemose, capillary, cavernous, and venous, according to the size of their vascular spaces. Cavernous and venous hemangiomas have low blood flow, because they lack arterial or capillary components. Histopathologically, venous hemangiomas contain dilated vessels with thick, fibrous walls, whereas cavernous hemangiomas have capillary-sized vessels lined by flat endothelial cells. A venous hemangioma involving the parapharyngeal space is an extremely rare vascular tumor. We report the first case of a venous hemangioma of the PPS and discuss its typical radiographic findings.
CASE REPORT
A 49-year-old female patient was referred for evaluation of swelling in the right submandibular region. She had swelling for the first time 3 weeks earlier, and it had not improved after medical treatment. She denied any history of trauma, fever, or surgery. Clinical examination revealed a soft mass in the right submandibular region and a bulge at the right lateral pharyngeal wall. A contrast-enhanced computed tomography (CT) scan revealed a cystic lesion, 4.6×3.0 cm, with contrast non-enhancement in the parapharyngeal space (PPS). There were several nodular calcifications within the cystic lesion (Fig. 1A). MRI showed a well-circumscribed non-enhancing mass with high signal intensity on T2-weighted images (Fig. 1B, C). A fine-needle aspiration biopsy was performed, but the report was inconclusive. A presumptive diagnosis of PPS dermoid cyst was made by a radiologist. The cystic lesion of the PPS was surgically removed using a transcervical approach. During surgery, numerous vessels were seen surrounding the mass. The lesion bled profusely, but the mass was bluntly dissected from the surrounding structures. The surgical specimen, measuring 4.3×4.5×2 cm, showed a pale-to-dark brown soft cut surface with a blood-filled spongy vascular lesion. Several hard bodies within the mass were observed. Microscopic examination revealed blood-filled sinusoidal spaces with large irregular lumens and thick walls lined by endothelial cells (Fig. 2A). Thick muscular blood vessels contained calcification and thrombus (Fig. 2B). This confirmed the diagnosis of a venous hemangioma. Postoperative recovery was uneventful, and there has been no evidence of cranial nerve palsy or tumor recurrence after one year.
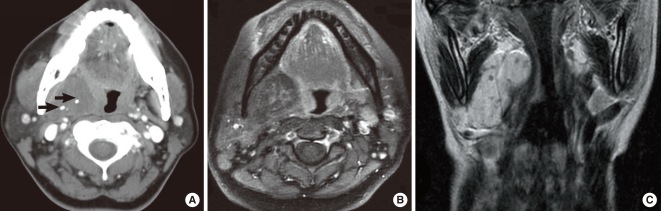
(A) Contrast-enhanced axial computed tomography scan shows a well-defined and hypoattenuating lesion, 4×3 cm in size, with two spotty calcifications (arrows), on the right parapharyngeal space. (B) The lesion shows low signal intensity on contrast-enhanced axial T1-weighted magnetic resonance images, and the three central areas of low signal intensity with peripheral rim enhancement correspond to the calcifications. (C) T2-weighted coronal magnetic resonance imaging shows that this lesion is hyperintense, making it easier to delineate from adjacent normal soft tissue.
DISCUSSION
PPS has a complex anatomy and close proximity to vital anatomical structures, with which it may become involved by various pathological processes. Presenting symptoms of PPS tumors may be attributed to the size of the mass and compression of neighboring structures (1). We had difficulty with the preoperative diagnosis, due to the absence of typical symptoms or signs of a vascular lesion in the PPS, such as pulsation or bruit. Fine-needle aspiration cytology (FNAC) was also not helpful in reaching a diagnosis. Although an exact tissue characterization of hemangioma in the PPS could not be made on FNAC, contrast-enhanced CT and magnetic resonance imaging (MRI) should be included in differentiating these lesions from other tumors of the PPS. In general, MR imaging is superior to CT imaging in its ability to ascertain the soft tissue characteristics of PPS tumors (2).
Cavernous and venous hemangiomas contain tortuous vascular channels with stagnant blood flow. Changes in the blood flow dynamics within a hemangioma result in thrombus formation and phleboliths (3). Phleboliths are calcified nodules that can be regarded as a characteristic property of venous or cavernous hemangiomas. CT with contrast is an excellent imaging technique for revealing phleboliths. Although MRI is not sensitive for the detection of small amounts of calcification, large amounts of calcification show discrete low signal intensity on all pulse sequences. MRI can produce high signal intensities, representing the blood, as well as focal heterogeneities, representing areas of thrombosis, fibrosis, or calcification (4). Although MRI is very useful for the detection of vascular lesions, the detectability of phleboliths on CT images is superior to that by MRI. Some reports have shown that plain X-ray films may also reveal calcified lesions.
When imaging shows calcification in the PPS, the differential diagnosis may include pleomorphic adenoma of the deep lobe of the parotid gland and metastatic thyroid carcinoma of the PPS. Pleomorphic adenoma with foci of chondroid or osteoid stroma can demonstrate opacities on imaging, but usually shows minute, scattered flecks. Additionally, in cases of metastatic thyroid carcinoma of the PPS, large flocculent calcification is seen on CT images (5).
Venous hemangioma cannot be clinically or radiologically differentiated from cavernous hemangioma, because of their similar characteristics. However, perfusion and blood pool scintigraphy has been demonstrated to have high sensitivity for detecting head and neck hemangioma, and can also differentiate between cavernous and venous hemangiomas (6).
Most venous hemangiomas are best treated by complete surgical excision. They tend to be larger and less well circumscribed, and show no tendency to regress (7). Attention needs to be given to the tumor location, extent, growth rate, and accessibility as well as the patient's age and esthetic concerns. The excision of large tumors in the PPS can be challenging, given the risk for severe hemorrhage and nerve injury. A surgical approach should be chosen according to the tumor size and location, its relationship to the great vessels, and any suspicion of malignancy. Generally, hemangiomas in the PPS, including venous hemangioma, can be resected by using a transcervical approach. Profuse bleeding often occurs during surgery, but after all of the pathology has been removed, the bleeding will cease. When surgery is impossible, the use of corticosteroids, cryotherapy, feeding vessel ligation, embolization, and fibrosing agents can be considered as alternatives (8).
In summary, we present the first reported case of venous hemangioma occurring in the parapharyngeal space. Considering that a presumptive diagnosis of most PPS tumors can be made based on imaging studies, preoperative imaging findings are very important in approaching these lesions. It may be that multiple, spotty, calcific nodules, 13 mm in size, within a cystic lesion on CT images indicate the pathognomonic finding of hemangioma in the PPS.
Notes
No potential conflict of interest relevant to this article was reported.
