Significance of the Extracapsular Spread of Metastatic Lymph Nodes in Papillary Thyroid Carcinoma
Article information
Abstract
Objectives
The extracapsular spread (ECS) of metastatic lymph nodes is associated with aggressive tumor behavior, and is regarded as a major risk factor for local recurrence in patients with head and neck squamous cell carcinoma. However, the significance of ECS of metastatic lymph nodes has not been well established in well-differentiated thyroid carcinoma. The purpose of this study was to examine this question.
Methods
A retrospective review was performed of 335 patients with papillary thyroid carcinoma who underwent total thyroidectomy with lymph node dissection from April 2001 to December 2009. We analyzed various clinical characteristics, pathologic factors, and the size, number, and ECS of foci in metastatic lymph nodes.
Results
On pathologic review, 201 of the patients (56.6%) had lymph node metastasis. This was significantly related to age and tumor size. ECS was noted in 64 of these 201 patients (31.8%), and was significantly related to male gender, tumor size, presence of extrathyroidal extension, metastatic lymph node size, and focus size. Recurrence occurred in 13 patients (3.9%), and the presence of ECS was significantly related to recurrence.
Conclusion
ECS of metastatic lymph nodes is an important prognostic factor for loco-regional recurrence in papillary thyroid carcinoma.
INTRODUCTION
Papillary thyroid carcinoma (PTC) is the most common malignancy of the thyroid. It has a good prognosis due to its slow growth and less invasive behavior [1]. However, lymph node (LN) metastasis or aggressive behavior, such as local invasion and distant metastasis are seen in some cases of PTC. Cervical LN metastasis is common in PTC; it is associated with recurrence and is a prognostic factor in older patients [23].
Microscopic examination of metastatic LNs can establish whether tumor foci are located within LNs with intact nodal capsules, or extend in to the surrounding perinodal fat tissue beyond the fibrous capsules of the LNs. In patients with head and neck squamous cell carcinoma, extracapsular spread (ECS) is associated with aggressive tumor behavior, and is regarded as a major risk factor for local recurrence [45]. However, in well-differentiated thyroid carcinoma, the significance of ECS has not been well established.
We hypothesized that ECS of metastatic LN may affect the prognosis of PTC. The purpose of this study was therefore to determine the clinical significance of ECS of metastatic LN in PTC.
MATERIALS AND METHODS
We retrospectively reviewed the data of 722 patients who underwent thyroidectomy for the treatment of PTC from April 2001 to November 2009. We confined this study to patients who underwent total thyroidectomy and LN dissection including central or lateral neck dissection. We excluded patients who did not receive neck dissection or total thyroidectomy, and had distant metastasis before operation, as well as recurrent cases. Finally, 335 patients were enrolled. The study was approved by the Institutional Review Board of Hanyang University Hospital (HYUH 2013-12-008-003).
Preoperative imaging was performed by neck ultrasonography (US) and computed tomography (CT), and in some cases, fluorine-18-fluorodeoxyglucose positron emission tomography/computed tomography (18FDG-PET/CT).
We analyzed various clinicopathologic characteristics, the size and number of metastatic foci, and ECS in metastatic LNs. Pathologic review was undertaken by two expert pathologists in our institution. Tumor size was defined by the length of the long axis of the largest nodule, and ECS by the existence of tumor foci that extended into the perinodal fat tissue surrounding the fibrous capsule of the LN (Fig. 1). Positive ECS patients were those who had ECS of one or more LNs.

Pathologic findings of lymph node metastasis in papillary thyroid carcinoma (H&E, ×40). (A) Metastatic tumor foci with intact lymph node capsule. (B) Metastatic tumor foci extend to the surrounding perinodal fat tissue beyond the fibrous capsule of the lymph node.
Clinically positive LN was defined as LN detected by palpation or preoperative image study such as US, CT, or 18FDG-PET/CT. We did not perform prophylactic neck dissection in the lateral compartment. We only performed therapeutic lateral compartment neck dissection when LN metastasis was suspicious clinically or LN metastasis was confirmed by US-guided fine needle aspiration cytology.
Tumors were classified according to 7th edition of the American Joint Committee on Cancer (AJCC) Staging System [6]. Local recurrence was evaluated every 6-12 months by neck US, radioactive iodine scan and stimulated serum thyroglobulin levels.
Statistical analysis was performed using IBM SPSS ver. 21.0 (IBM Co., Armonk, NY, USA). Pearson chi-square test, Fisher exact test, or the independent t-test was used in evaluating the relation between local recurrence and various clinical factors, as well as between ECS and various clinical factors. After identifying significant clinical factors, a multiple regression analysis was performed to identify risk factors related to local recurrence and ECS.
RESULTS
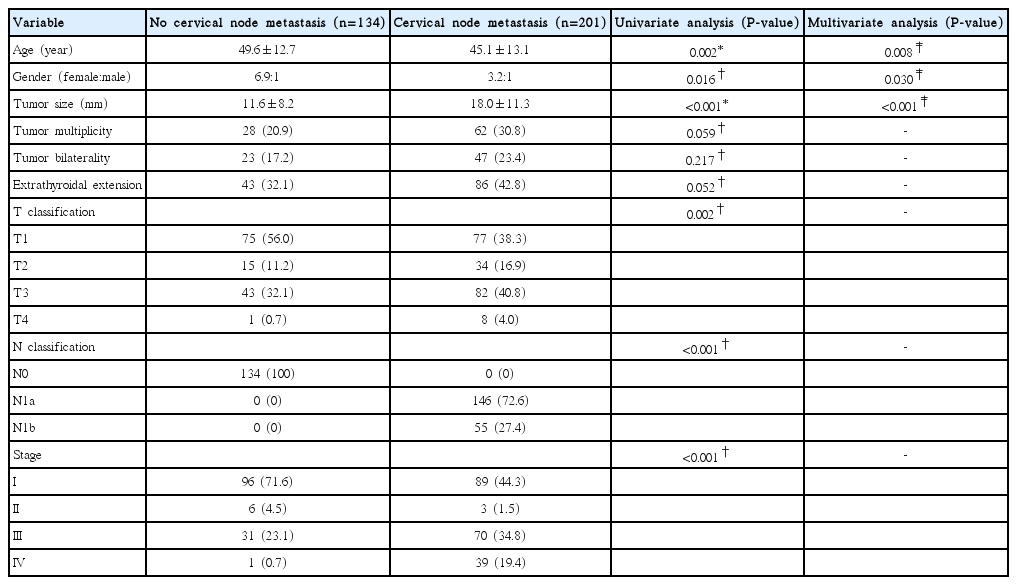
The mean age of the 335 patients was 46.9 (standard deviation, ±13.1) years, and 80.6% were female. Pathologic cervical LN metastasis was found in 201 patients (56.6%). According to the AJCC staging system, the numbers of patients in stages I, II, III, and IV were 185 (55.2%), 9 (2.7%), 101 (30.1%), and 40 (11.7%), respectively. Postoperative radioactive iodine ablation was performed in 306 patients (91.3%), and the mean follow-up period was 69.0 months (range, 33 to 147 months). Factors related to LN metastasis are listed in Table 1. Cervical LN metastasis was related to age, gender, and tumor size (P=0.008, P=0.030, and P<0.001, respectively).
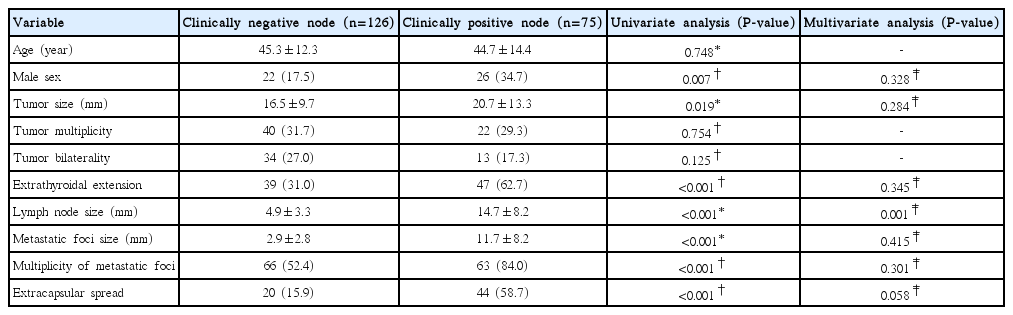
Of 201 patients with cervical LN metastasis, the proportions of LNs that were detected by preoperative physical examination or imaging were 13.7% (20/146) and 100% (55/55) in central and lateral compartment, respectively. A comparison between the clinically positive and the clinically negative LN groups is shown in Table 2. Metastatic LN detected clinically was related to metastatic LN size (P=0.001).
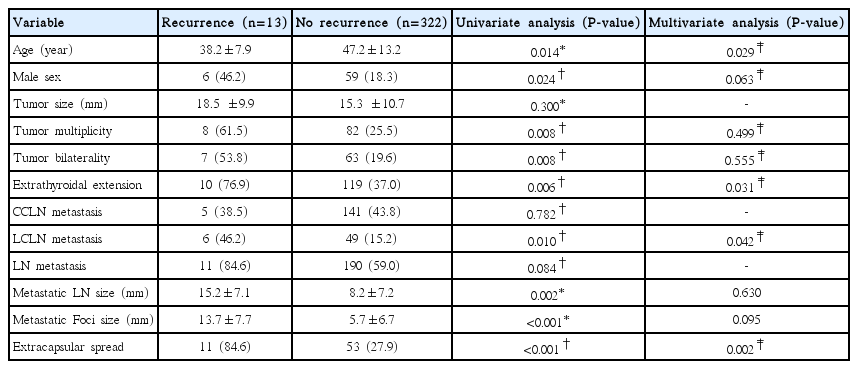
Pathologic review of the 201 patients with cervical LN metastasis showed that 64 (31.8%) had ECS. Positive ECS was significantly related to male gender, tumor size, and extrathyroidal extension (ETE) (Table 3).

Factors related to extracapsular spread (ECS) of metastatic lymph nodes in papillary thyroid carcinoma
ECS was found in 242 of the total of 1,121 LNs (21.6%) removed in all patients. It was seen in 11.0% (49/445) and 28.6% (193/676) of the LNs in the central and lateral LN metastasis groups, respectively. The relationship between ECS and nodal characteristics is detailed in Table 4. Larger metastatic LN size and focus size were independent risk factors for ECS in multivariate regression analysis (P<0.001, each).
Recurrence in cervical LNs occurred in 13 patients (3.9%); two in the group without LN metastasis and eleven in the group with positive LN metastasis. There was no recurrence in the thyroid bed or other organs. Gender, tumor size, multiplicity, bilaterality, central LN metastasis, metastatic LN size, and metastatic foci size were not significantly related to loco-regional recurrence. On the other hand, lower age, presence of ETE, lateral LN metastasis, and ECS were risk factors for loco-regional recurrence in multivariate regression analysis (Table 5). In a subgroup analysis of the cases with cervical LN metastasis, loco-regional recurrence was significantly associated with age and presence of ECS (Table 6). Radioactive iodine ablation did not significantly influence local recurrence (P=0.394).
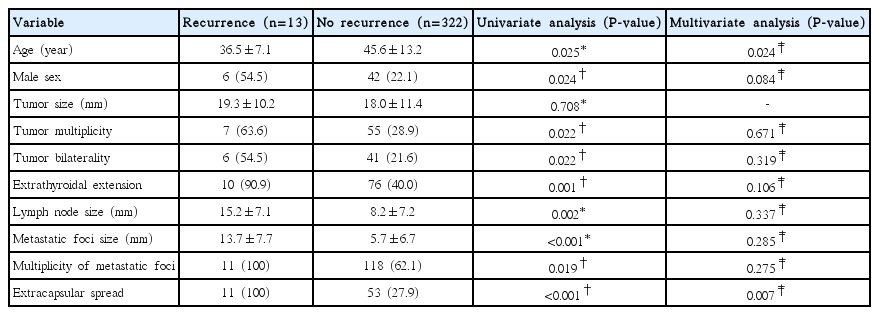
Factors related to loco-regional recurrence in papillary thyroid carcinoma with lymph node metastasis
In the group of patients who underwent only central neck dissection, the site of LN recurrence was the central compartment in one case, the lateral compartment in five cases, and both central and lateral compartment in one case. In the group who underwent lateral neck dissection, the site of LN recurrence was the central compartment in two cases and the lateral compartment in the other four.
DISCUSSION
Rates of cervical LN metastasis in PTC vary. The frequency of cervical LN metastasis was reported to be 20%-41% as detected clinically by preoperative physical examination, US or CT, whereas pathologically confirmed cervical LN metastasis occurred in 20%-80% of cases [78910]. In this study, 22.4% of the patients (75/335) had clinically detectable LN metastasis by physical examination or imaging study while 60.0% (201/335) had LN metastasis confirmed pathologically after surgery. According to several studies, cervical LN metastasis is related to lower age, large tumor size, presence of ETE, and positive BRAF V600E mutation [111213]. In this study, lower age, male gender, and large tumor size were associated with increased cervical LN metastasis.
Cervical LN metastasis in differentiated thyroid carcinoma has no definite effect on prognosis, but is a critical factor for local recurrence [14]. In this study, young age, ETE, lateral LN metastasis, and ECS of metastatic LNs were significantly related to loco-regional recurrence.
The size and number of metastatic LNs is thought to be associated with local recurrence although this is controversial [111516]. In this study, the size of metastatic LNs was not significantly correlated with loco-regional recurrence.
Several studies have concluded that ECS of metastatic LNs is related to lower age, large tumor size, presence of ETE, and size and number of metastatic LNs [11121718192021]. T4 tumors and high-risk features according to the American Thyroid Association guidelines were associated with ECS of metastatic LNs [19]. In this study, ECS of metastatic LNs was related to male gender, large tumor size, presence of ETE, large size of metastatic LNs and large size of metastatic foci.
ECS of metastatic LNs is regarded as a poor prognostic factor for local recurrence and survival in some human cancers such as head and neck, breast and bladder cancers. ECS of metastatic LNs, especially in head and neck cancers, is considered an important adverse prognostic factor for local recurrence and distant metastasis, as well as for survival [45].
There are differing opinions about the significance of ECS in PTC. Several studies have reported it to be a prognostic indicator for local recurrence, distant metastasis, and decreased survival [11121718192021]. A recent paper concluded that the risk of recurrence was 1% in patients with LN metastasis without ECS, 4% in those with three metastatic LNs showing ECS, and 32% in those with more than three metastatic LNs showing ECS [11]. According to another study more than three metastatic LNs showing ECS was also a significant risk factor for persistent disease and recurrent disease [20]. In addition, concurrent BRAF V600E mutation and ECS of metastatic LNs have been shown to predict significantly worse disease free survival [18]. However, in other studies workers found that recurrence was not correlated with ECS of metastatic LNs [2223].
In our study, ECS of metastatic LNs was significantly associated with loco-regional recurrence. Young age and presence of ECS, in particular, were significantly associated with recurrence among patients with cervical LN metastasis. Therefore, close postoperative surveillance and appropriate adjuvant treatment should be considered in patients with ECS in order to detect early recurrence and minimize loco-regional recurrence. In this study, only two patients died. ECS of metastatic LNs was not correlated with survival although the follow-up period was relatively short to evaluate survival rate accurately.
In conclusion, ECS of metastatic LNs in PTC is an important prognostic factor for loco-regional recurrence.
Notes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.