Is Ginger Effective in Reducing Post-tonsillectomy Morbidity? A Prospective Randomised Clinical Trial
Article information
Abstract
Objectives
An assessment of the effects of ginger on pain, nausea, vomiting, bleeding, and wound site healing that occur after tonsillectomy.
Methods
This prospective clinical study was participated by 49 patients aged 18–45 years out of 56 patients that underwent tonsillectomy and regularly attended follow-up visits. The patients were randomly divided into two groups. Group 1 consisted of 23 patients that used ginger capsules and group 2 consisted of 26 patients that did not use ginger capsules in addition to the routine antibiotic and paracetamol treatment following tonsillectomy. The pain, nausea, vomiting, and bleeding scores of patients were assessed on days 1, 4, 7, and 10 by using the visual analogue scale. Similarly, the epithelialization degrees of tonsillar bed were assessed on postoperative days 1, 4, 7, and 10 and regular oral intake times of patients were recorded.
Results
There were no differences between groups in terms of age and sex. On the postoperative days 1, 4, 7, and 10, the pain scores were lower in the group 1 (all P<0.001) and there were no differences between the two groups in terms of postoperative nausea, vomiting, and bleeding scores (P=0.35 and P=0.53). On the postoperative days 7 and 10, epithelialization in the tonsil bed was quicker in the group 1 (P=0.041 and P=0.026) and the regular oral intake time was earlier in group 1 (P<0.001).
Conclusion
In this study, ginger relieved pain, accelerated wound site epithelialization, and decreased duration of oral intake following tonsillectomy. It did not result in postoperative bleeding or any other complications. Ginger can be recommended as an adjunct to routine medical treatment for decreasing morbidity following tonsillectomy.
INTRODUCTION
Tonsillectomy is globally one of the most frequently performed surgeries on children and adults. Even though we currently have advanced surgical techniques, patients often complain about postoperative nausea, vomiting, throat ache, and consequent decrease in oral intake. The reasons for this pain include secondary healing of the wound site, inflammation, pharyngeal muscle spasm and glossopharyngeus and vagus nerve irritation. The pain persists until approximately 2–3 weeks as the pharyngeal muscles are covered by the mucosa. In order to relieve postoperative pain following tonsillectomy, several methods and medical therapeutic agents have been used such as hyaluronic acid [1], magnesium [2], opioid [3], honey intake [4], sucralfate in the tonsil region [5], and autologous serum [6].
Ginger, which is scientifically known as Zingiber officinale, is a plant that has anti-inflammatory and analgesic properties known in many Asian countries [7]. The anti-inflammatory property of ginger originates from compounds such as gingerols, shogaols, and paradols in its composition. Studies performed have also shown that ginger not only brings about lipoxygenase inhibition, thereby reducing the synthesis of inflammatory leukotrienes [8], but it also shows an anti-inflammatory effect by enabling cytokine inhibition in a way similar to betamethasone [9].
Additionally, studies conducted have also shown that ginger is effective in enhancing wound healing [10,11], preventing postoperative nausea and vomiting (antiemetic) [12], relieving pain due to dysmenorrhea [13-15], osteoarthritis [16], and rheumatoid arthritis [17]. As can be seen, there are several studies where ginger has been clinically applied, however, our literature review did not show any studies investigating the intake of ginger for pain and morbidity that develop after tonsillectomy. The aim of this study is to investigate the effects of ginger on pain following tonsillectomy and to ensure that patients begin oral intake in a shorter period of time following the operation.
MATERIALS AND METHODS
The study was initiated after the approval was obtained from the Kocaeli University Clinical Research Ethics Committee (approval No. 4/15). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the Helsinki declaration and its later amendments or comparable ethical standards. Our study included 56 patients aged 18–45 years, who received the indication for tonsillectomy due to recurrent tonsillitis, snoring due to tonsillar hypertrophy or chronic tonsillitis resistant to medical treatment between September 2015 and February 2017. Patients who previously underwent tonsillotomy, underwent another surgery simultaneously with tonsillectomy (such as uvulopalatopharyngoplasty or other snoring surgeries), had mental retardation, had to continuously use painkillers, and had known allergy to ginger were excluded from the study. Written and oral informed consents were obtained from the patients prior to the study. The patients were randomly divided into two groups by a department nurse on the day of surgery. Tonsillectomy was performed by a surgeon under general anesthesia using the conventional cold dissection technique. Bleeding control was done using a bipolar cautery. Patients in group 1 (n=28) were administered amoxicillin/clavulanate (1,000 mg) two times per day, paracetamol tablets (500 mg) three times per day, and ginger capsules (500 mg; Ginger Root, Solgar, Leonia, NJ, USA) two times per day for 7 days postoperatively. Patients in group 2 (n=28) were administered amoxicillin/clavulanate (1,000 mg) two times per day, paracetamol tablets (500 mg) three times per day for 7 days postoperatively. The patients did not know that the ginger capsules had analgesic properties. The patient’s pain was evaluated on days 1, 4, 7, and 10 by an otorhinolaryngologist who was unaware of the procedure on the basis of visual analogue scale (0, no pain; 10, severe pain).
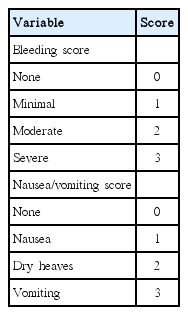
Postoperative nausea, vomiting, and bleeding complaints were evaluated by an otorhinolaryngologist who was unaware of the procedure on days 1, 4, 7, and 10 on the basis of the scale in Table 1 [2]. Epithelialization in the tonsillar bed was also evaluated by an otorhinolaryngologist who was unaware of the procedure on days 1, 4, 7, and 10 using the method previously defined in the literature (Table 2) [4]. The patients were recommended to have a soft diet in the first week. Furthermore, they were asked on which postoperative day they began regular oral intake.
Statistical analysis
Statistical analysis was carried out using IBM SPSS ver. 22.0 (IBM Corp., Armonk, NY, USA). All the quantitative variables were estimated using measures of central location (i.e., mean and median) and measures of dispersion (i.e., standard deviation). Data normality was checked using the Kolmogorov-Smirnov tests of normality.
Mann-Whitney U-test and independent t-test were used in between-group evaluation for quantity data (age, pain scores, bleeding scores, nausea/vomiting scores, time to regular oral intake).
Chi-square test was used for the comparison of qualitative data (gender, degree of epithelialization). A P-value <0.05 was considered statistically significant.
RESULTS
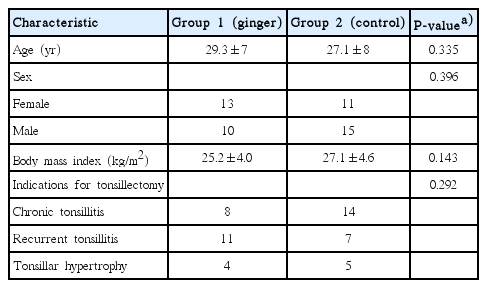
The study included 56 patients (31 males and 25 females, aged 18 to 45 years) who underwent tonsillectomy surgery. Out of these patients, seven patients (five patients in group 1 and two patients in group 2) did not regularly attend their follow-up visits. Group 1 (n=23) had 10 male and 13 female patients between 21 and 45 years (average, 29.3±7 years) of age. Group 2 (n=26) had 15 male and 11 female patients between 18 and 39 years (average, 27.1±8 years) of age. There were no statistically significant differences between two groups in terms of gender, age, body mass index, and indication for tonsillectomy (Table 3).
When the groups were compared in terms of pain score, it was seen that the pain score of the group that took ginger (group 1) was lower than that of the group 2 on postoperative on days 1, 4, 7, and 10 (all P<0.001) (Fig. 1). This is an indication that patients who take ginger following tonsillectomy have less pain during the postoperative period.

Comparison of pain visual analog scale scores on postoperative (postop) days 1, 4, 7, and 10. Vertical error bars represent standard error. ***P<0.001.
Even though bleeding was observed in two patients in group 2 on postoperative days 3 and 8, there are no statistical differences between the two groups in terms of bleeding scores (P>0.05). As can be seen here, ginger did not negatively influence bleeding. Additionally, no significant differences were seen between the two groups on postoperative days 1, 4, 7, and, 10 with respect to the vomiting and nausea scores (P>0.05).
When the degree of epithelialization in the tonsillar bed was compared, there were no differences between the two groups on postoperative days 1 and 4 (all P>0.05) while it was seen that epithelialization was better in the group 1 on postoperative days 7 and 10 (P=0.041 and P=0.026) (Fig. 2, Table 4). Seventy-four percent of patients in group 1 and 42% of patients in group 2 showed grade 4 epithelialization on day 10. Judging from this result, it could be suggested that ginger accelerates wound healing in line with the literature data [10,11].
Representative view of tonsillar bed at postoperative day 10. (A) Patient who took ginger, (group 1), (B) patient who did not take ginger (group 2).
The regular oral intake time of the patients in group 1 was postoperatively 3.2±0.6 days, while this was observed to be 4.6±0.9 days for group 2. The patients who took ginger began oral intake at an earlier stage (P<0.001).
DISCUSSION
Throat ache is a complaint that frequently develops following tonsillectomy surgery and it may lead to undesired situations such as prolonged hospitalization, poor oral intake, dehydration, and late return to daily life. In the past, several agents were used to relieve pain following tonsillectomy [1-6] and they each have individual advantages and disadvantages. For that reason, there is currently not a consensus on relieving pain after tonsillectomy. Opioids and nonsteroidal anti-inflammatory drugs (NSAIDs) are the drugs that are most frequently used to relieve pain after tonsillectomy. As it is well-known, opioids may lead to respiratory depression and sedation. As for NSAIDs, they are commonly used even though their use is still controversial since they have effects on platelets and prolong bleeding time [18]. Paracetamol is a reliable drug to be taken after tonsillectomy; however, it is not adequately effective against throat ache and its use at a high dose may result in hepatotoxicity [19].
Ginger, which is more often used globally to add flavor to dishes is a plant known in Asian countries with its anti-inflammatory and analgesic properties. Shirvani et al. [13] and Rahnama et al. [14] showed that ginger reduced pain related to dysmenorrhea. Ozgoli et al. [15] reported that ginger was as effective as mefenamic acid and ibuprofen as a painkiller. Bartels et al. [16] showed that ginger was effective in treating osteoarthritis-related pain and Al-Nahain et al. [17] showed that it was effective in symptomatic treatment of pain associated with rheumatoid arthritis. Similarly, it was stated in the literature that ginger was effective against throat ache [20]. Ginger enables cyclooxygenase and lipoxygenase enzyme inhibition through the arachidonic acid metabolism. Consequently, it shows analgesic and anti-inflammatory effects by ensuring prostaglandin and leukotriene suppression [14]. In another mechanism, it shows an anti-inflammatory effect via cytokine inhibition in a way similar to betamethasone [9]. In conclusion, it has been used to control pain in several diseases as seen. However, we have not found any studies in the literature that investigated the efficacy of ginger in relieving pain following tonsillectomy. In the line of these studies, we considered that ginger could relieve postoperative pain following tonsillectomy. In the study that we conducted, we observed that patients who took ginger after tonsillectomy had less pain on postoperative days 1 to 10 as compared to patients who did not take it (postoperative days 1,4,7,10; P<0.001). Judging by this result, it could be concluded that ginger helps relieving pain that develops after tonsillectomy.
Studies in the literature have shown that ginger is effective against postoperative nausea and vomiting [12,21]. The mechanism of action here is not entirely clear. Some authors advocate that it shows an antiemetic effect by reducing stomach contractions and increasing the intestinal system activity [21], while other authors state that it prevents nausea and vomiting by having an inhibitory effect on 5-HT serotonin receptors in a way similar to antiemetic drugs. We also investigated the effect of ginger on nausea and vomiting after tonsillectomy; however, we did not see any differences between the two groups in terms of postoperative nausea and vomiting (P>0.05). We believe that we could not see a significant difference since the patients took ginger after the operation in our study, whereas ginger was given approximately 1 hour before the operation to patients for postoperative antiemetic effect in the studies performed [12,21].
Several studies investigated the effects of ginger on coagulation. Jiang et al. [22] reported that ginger showed an anticoagulant effect in a way similar to aspirin. In another study, it was demonstrated that ginger did not have any effects on platelet aggregation [23]. Additionally, Kashefi et al. [24] showed that ginger reduced menstrual bleeding in a study that they conducted. In our study, none of the patients that took ginger had bleeding. Postoperative bleeding was observed in two patients in the group that did not take ginger, although there were no statistically significant differences between the two groups in terms of postoperative bleeding. Based on this result, it could be suggested that ginger does not have any side effects related to bleeding.
Another property of ginger is that it accelerates wound healing. In two experimental studies, it was demonstrated that ginger contributed to the enhancement of wound healing [10,11]. The role of ginger in wound healing has not been entirely understood. It was considered that this could be because it supported blood vessel formation in the healing tissue and increased the level of type 1 collagen [11]. We also saw in our study that the tonsillar bed epithelialization was statistically significantly better in patients that took ginger on postoperative days 7 and 10 as compared to those who did not take it (Fig. 2). We can conclude that ginger accelerates healing in the tonsillar bed.
Delayed begin to oral intake and consequent dehydration are complications that may develop after tonsillectomy. Early begin to oral intake after tonsillectomy is important in the sense that it ensures that patients recover rapidly and shortens the hospital stay. In this study that we conducted, we saw that patients taking ginger began oral intake at an earlier stage (P<0.001). We believe that they started regular oral intake earlier because patients taking ginger have less postoperative pain.
Rahnama et al. [14] reported in their study that some subjects who took ginger had side effects such as heartburn. In the study by Rahnama et al., heartburn may have arisen out of the use of ginger at a high dose. In our study, patients taking ginger did not have any gastrointestinal effects such as heartburn and similar issues. Furthermore, bleeding, which is a potential side effect of ginger, was not seen in patients taking ginger in our study, either. This is probably due to the fact that we used ginger at a lower dose.
The studies have shown that ginger was as effective as ibuprofen (NSAID) the management of pain after dental surgery [25] and in patients with osteoarthritis [26], also as effective as ibuprofen and mefenamic acid in relieving menstrual pain [13,15]. Furthermore, ginger has been accepted as safe by both the Food and Drug Administration [7] with no report of severe side effects or drug interactions in Germany’s Commission E Monograph [27]. In contrast, adverse effects of NSAIDs include gastrointestinal disorders (such as nausea, dyspepsia, and vomiting) and central nervous system symptoms, nephrotoxic and hepatotoxic effects, hematological abnormalities, and bronchospasm [13]. Sometimes, tonsillectomy is associated with nausea and vomiting. Although NSAIDs may lead nausea and vomiting, ginger also alleviates these symptoms [12,21]. Ginger may be preferred for patients who do not want to use NSAIDs because of its adverse effects.
Considering cost of ginger capsule, its price is about $14 (for 60 capsules). Although the costs of different NSAID agents vary, average price of NSAID drugs are approximately $10 (for 20 tablets). Ginger capsules are not more expensive than NSAIDs analgesics. Also, ginger can reduce postoperative pain and consequently the need for extra analgesic consumption. Furthermore, ginger may reduce the treatment costs due to the side effects of NSAIDs (such as bleeding and gastrointestinal problems) or the length of stay in the hospital because of late oral intake. For all these reasons, we think that ginger can be cost-effective for postoperative management. We currently recommend patients undergoing tonsillectomy to take ginger alongside analgesic drugs such as paracetamol for pain control and we receive positive feedback.
One of the limitations of our study is that the sample size is small even though it is statistically adequate. In the future, studies with several patients’ groups and multiple centers may be conducted. Another limitation is related to the dose of ginger. There is not an existing consensus on the maximum dose of ginger per day. Even though maximum daily dose is considered to be 2 g in Europe and America, the daily dose goes up to 9 g in Asia [28]. We determined the dose of ginger in the study we conducted by referencing the previous studies in the literature. Also, other limitations of the study could be attributed to an absence of placebo or other NSAIDs treatment in the control group. Although our study lacked a placebo group, it was still prospectively randomized controlled study and compared the treatment group with a relevant control group and as such has a low risk of bias. Placebo-controlled or comparative studies are needed to support our findings and minimize bias in data collection.
This study has shown that ginger has facilitated pain management following tonsillectomy. Additionally, patients who took ginger had a faster tonsil bed epithelialization and an earlier begin to regular oral intake. Also, no side effects were observed. For that reason, we recommend patients to take ginger alongside analgesic drugs such as paracetamol following tonsillectomy. However, studies with larger sample sizes and multiple centers are needed to support our results and to demonstrate the efficacy of ginger against post-tonsillectomy morbidities.
HIGHLIGHTS
▪ Ginger relieved pain, accelerated wound site epithelialization, and decreased duration of oral intake following tonsillectomy.
▪ Ginger did not result in postoperative bleeding or any other complications.
▪ Ginger can be recommended as an adjunct to routine medical treatment for decreasing morbidity following tonsillectomy
Notes
No potential conflict of interest relevant to this article was reported.