Pre-operative Evaluation of Eustachian Tube Function Using a Modified Pressure Equilibration Test is Predictive of Good Postoperative Hearing and Middle Ear Aeration in Type 1 Tympanoplasty Patients
Article information
Abstract
Objectives
The Eustachian tube (ET) plays an important role in maintaining a normally aerated middle ear. Inflammation in middle ear disease is related to ET dysfunction, and postoperative restoration of middle ear integrity and hearing are closely related to ET function in chronic ear disease patients. After successful tympanoplasty, restoration of a well-aerated middle ear with good ET function can permit better compliance of the tympanic membrane. In this study, we evaluated the predictive validity of preoperative ET function measurements.
Methods
We reviewed 137 patients who underwent type 1 tympanoplasty. All patients had non-cholesteatomatous chronic otitis media and received canal wall-up-type tympanomastoidectomies. Patients were categorized into four groups according to preoperative ET function measurements using a modified pressure inflation-deflation equilibration test. Group I patients had residual pressures less than 10 daPa, and Group IV patients showed no pressure change (poor results). Groups II and III were intermediate. Hearing levels were determined using pure tone averages at four frequencies. Postoperative tympanography was performed to determine middle ear aeration.
Results
The preoperative air bone (AB) gap was 29.6±7.0 dB, and the postoperative gap was 16.5±5.7 dB; thus, there was significant overall improvement. In all groups, hearing was significantly better after surgery, but the worst postoperative hearing level was seen in Group IV patients. Type B tympanograms were more frequently recorded in Group IV patients than they were in Group I or II patients. Postoperative AB gaps were 9.2±3.8 dB in patients with type A tympanograms, 13.4±2.1 dB in those with type As, 24.1±2.5 dB in those with type C, and 18.5±2.8 dB in those with type B.
Conclusion
ET function measured with a modified pressure equilibration test using an inflation-deflation manometric method is a good indicator of an aerated middle ear and is predictive of improved postoperative hearing.
INTRODUCTION
The Eustachian tube (ET) plays an important role in maintaining normal aeration of the middle ear. Inflammation in middle ear disease is related to ET dysfunction, and postoperative restoration of middle ear integrity and hearing are closely related to ET function in patients with chronic ear disease (1). Better results after tympanoplasty have been reported in patients with normal ET function (2), and higher failure rates after tympanoplasty have been observed in patients with ET problems (3). It might therefore be possible to predict postoperative results such as hearing improvement and disease recurrence, and to choose optimal operative methods, if ET function can be assessed preoperatively.
Although no method for precisely measuring ET function has been reported to date (4), the Valsalva maneuver or inflation/deflation tympanometric tests have recently been used to predict postoperative results and to guide operative technique choice (5, 6). Takahashi and colleagues reviewed 78 patients with non-cholesteatomatous chronic otitis media, without ossicular damage. ET pressure-regulation functions were examined using an inflation-deflation test, and postoperative hearing levels were measured. Patients with poor pressure regulation showed a significantly higher incidence of poor outcomes, poor hearing recovery, spontaneous perforation of the tympanic membrane, or persistent wet condition (5). Uzun (6) reported 61 ears with tensa cholesteatoma in 60 children who underwent tympanoplasty with cartilage palisades or fasciae. These authors evaluated preoperative ET function using the Valsalva maneuver and found that late hearing results were better in patients with positive Valsalva maneuvers than they were in those with negative maneuvers. With respect to ears with poor tubal function, hearing results were significantly better in those treated with cartilage palisade tympanoplasty than they were in those treated with fascia reconstruction. The authors suggested that cartilage palisade tympanoplasty might be a better reconstruction option for patients with poor ET function.
A compliance (immittance) peak on a tympanogram indicates that the ear canal and middle ear pressures are equal, and that acoustic transmission through the middle ear is maximal. Tympanograms are classified with respect to this peak (7). After successful tympanoplasty, restoration of a well-aerated middle ear with good ET function can permit better compliance of the tympanic membrane, yielding an A-type tympanogram. However, no relationship between preoperative ET function and postoperative middle ear aeration has yet been reported.
In the present study, we measured preoperative ET function using a modified pressure equilibration test and postoperative middle ear aeration by impedance audiometry. We then evaluated the predictive validity of preoperative ET function measurements.
MATERIALS AND METHODS
In this study, we reviewed 137 patients who underwent type 1 tympanoplasty between 2004 and 2006. All patients had non-cholesteatomatous chronic otitis media and underwent canal wall-up-type tympanomastoidectomy. The temporalis fascia was used in tympanic membrane reconstruction. Patients with ossicular fixation or ossiculoplasty were excluded from this study. If granulation blocked a tympanic orifice or the ET, the granulation was removed and the orifice was re-opened. Data on clinical courses, intraoperative findings, hearing results, and impedance audiometry were collected and retrospectively analyzed. The study protocol was approved by the Institutional Review Board of Asan Medical Center.
Preoperative ET function was measured using a modified pressure equilibration inflation-deflation test (8). After confirmation of dryness of both the external and middle ear by otoscopy, a probe was fitted into the external auditory canal, and pressure was varied over ±300 daPa. Each patient was asked to swallow three times at intervals of 3-5 sec with nose and mouth closed. After each swallow, applied pressure was normalized, as shown in Fig. 1. The residual pressure after three swallows was recorded. ET function was evaluated and graded as shown below, with reference to residual pressure after each application of positive or negative pressure (9, 10):

Examples of recordings from the pressure equilibration test, showing residual pressure (Pr). Group I ears completely equilibrated to both positive and negative pressures (Pr<10 daPa and >-10 daPa, respectively). Group II ears partially equilibrated to both positive and negative pressures (Pr>10 daPa and <-10 daPa, respectively). Group III ears completely or partially equilibrated to positive pressure, but could not equilibrate to negative pressure. Group IV ears could not equilibrate to either positive or negative pressure.
Grade I: Residual pressure <±10 daPa after each pressure application
Grade II: Residual pressure <±10 daPa only after positive pressure application
Grade III: Residual pressure >±10 daPa, but pressure changed with swallowing after any pressure application
Grade IV: No change in pressure after any pressure application
The hearing level was determined by measuring pure tone averages at four frequencies (0.5, 1, 2, and 3 kHz), according to guidelines for the evaluation of treatment results for conductive hearing loss (11). Preoperative hearing was measured within three months before surgery. Postoperative hearing was measured, and tympanography was performed, three to six months after surgery. For tympanography, we used a probe with a soft plastic tip and delivered a probe tone of 226 Hz into the ear canal while varying air pressure in the external ear canal from +200 to -400 daPa. Tympanograms were classified into four types according to shape: A, As, C, and B (7).
RESULTS
Of the 137 patients, 79 were male and 58 were female. The average age was 46.2 yr (range, 35 to 65 yr). Postoperative follow-up periods ranged from 18 to 42 months with an average of 28.2 months. Patients were classified into four groups according to modified pressure equilibration test data: 24 patients in Group I, 26 in Group II, 31 in Group III, and 56 in Group IV. The overall mean preoperative AB gap was 29.6±7.0 dB, and the postoperative gap was 16.5±5.7 dB, thus showing significant improvement (paired t-test, P=0.002). Preoperative and postoperative AB gaps, respectively, were 27.3±7.5 dB and 13.9±5.9 dB in Group I, 27.2±7.0 dB and 14.1±6.3dB in Group II, 30.7±7.1 dB and 16.5±5.5 dB in Group III, and 31.0±6.3 dB and 18.6±4.5 dB in Group IV (Fig. 2). In all groups, hearing significantly improved after surgery. The mean postoperative hearing level was significantly worse in Group IV patients than it was in Group I or II patients (Fig. 2).
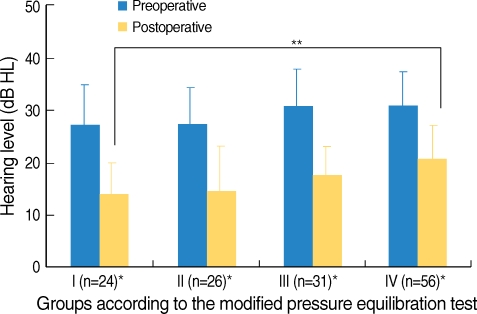
Mean preoperative and postoperative hearing levels of groups classified with respect to results of the modified pressure equilibration test.
*Postoperative hearing was better than preoperative hearing was in all groups (P<0.05). **The postoperative hearing of Group IV patients was significantly worse than that of Group I patients (P<0.01).
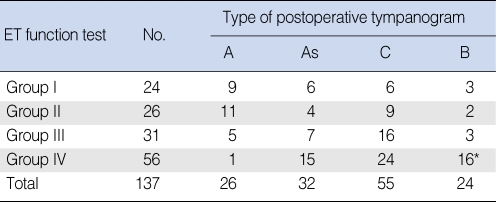
Postoperative tympanography showed type A traces in 26 patients, type As in 32, type C in 55, and type B in 24 (Table 1). Type B tympanograms were more frequently recorded in Group IV patients than they were in Group I or II patients (P<0.01, Spearman Chi Square test). The mean postoperative AB gap was 9.2±3.8 dB in patients with type A tympanograms, 13.4±2.1 dB in those with type As, 24.1±2.5 dB in those with type C, and 18.5±2.8 dB in those with type B (Fig. 3).
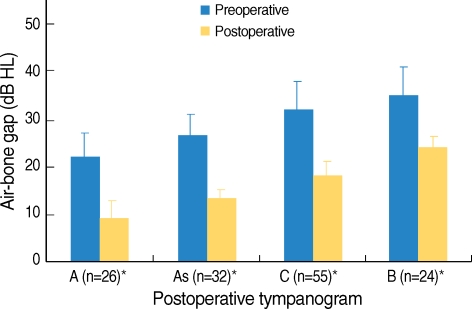
Preoperative and postoperative hearing levels of patients classified into different types with respect to postoperative tympanography.
*Postoperative hearing was better than preoperative hearing was in all patient types (P<0.05).
The hearing of patients with middle ear mucosal swelling and granulation tissue (n=51) was 35.8±4.8 dB preoperatively, but improved to 20.8±4.0 dB postoperatively. In patients with intact middle ear mucosa (n=86), hearing improved to 14.0±4.9 dB from 25.9±5.3 dB preoperatively. The mean postoperative hearing level was significantly better in patients with intact middle ear mucosa (Fig. 4).
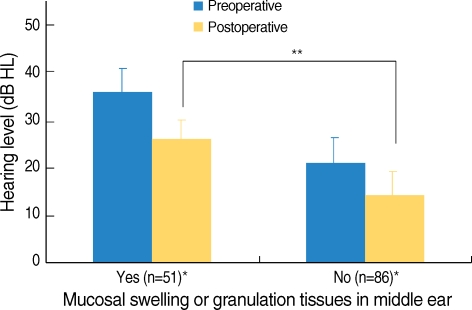
Preoperative and postoperative hearing levels of patients with or without middle ear mucosal swelling and granulation tissue.
*Postoperative hearing was better than preoperative hearing was in both groups (P<0.05). **The postoperative hearing level of patients with mucosal swelling and granulation tissue was significantly worse than that of patients without such complications (P<0.01).
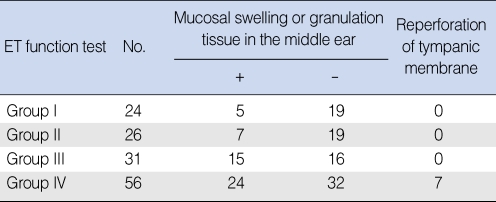
Mucosal swelling was more frequently found in Groups III and IV (Table 2). Tympanic membrane reperforation occurred postoperatively in 7 of 51 patients with middle ear mucosal swelling or granulation tissue, but in no patients without these complications. These seven patients were all in group IV, and all had type B tympanographies postoperatively (Table 2).
DISCUSSION
Because good ET function may enhance middle ear aeration, postoperative tympanic membrane mobility can be optimized to permit hearing improvement using the normal amplification mechanism of the middle ear. In the present study, we observed a mean hearing improvement of 11-14 dB regardless of ET functional status. However, the postoperative AB gap was worse in Group IV patients than it was in Group I or II patients. In addition, better ET function was related to an aerated middle ear, and patients with satisfactory ET status yielded type A tympanograms showing good membrane compliance.
Normal middle ear aeration is reflected in type A tympanography, whereas a thick tympanic membrane, middle ear effusion, or retraction of the tympanic membrane yields tympanography data of other types: As, C, and B (7). A type A tympanogram implies that middle ear volume is over 0.5-2.0 cm3 and aeration through the ET is undisturbed (12). Within this volume, the normal amplification mechanism of middle ear sound permits hearing improvement up to the normal value (9.2 dB).
For ventilation and pressure regulation within the middle ear, gas exchange via the middle ear mucosa and the mastoid is important, in addition to exchange via the ET. In the present work, 51 patients had mucosal swelling or granulation tissue in the middle ear cavity. A diseased mucosa can function as a barrier to normal gas exchange and can also block the ET directly. The hearing results were poorer in these patients than they were in those with intact middle ear mucosa. Because transmucosal gas exchange is passive and is caused by a partial pressure gradient between the middle ear cavity and the mucosal capillaries, such mucosal exchange is impaired by inflammatory changes in the middle ear mucosa and mastoid (13, 14). Furthermore, gas exchange via the mucosa seems to be less impaired than is gas exchange via the ET (14). The co-presence of middle ear mucosal swelling and granulation tissue is a poor prognostic sign, indicating interference with gas exchange both through the mucosa per se and the ET. The tympanic membrane reperforations in Group IV patients, and the B-type tympanograms obtained postoperatively, also support the idea that middle ear mucosal swelling and granulation tissue are poor prognostic signs. Overall, good ET function facilitates better hearing, improves restoration of middle ear aeration, and leads to fewer post-operative complications.
Accordingly, preoperative evaluation of ET function can be used in the planning of treatment and selection of surgical technique, such as epitympanic obliteration or cartilage tympanoplasty (6).
Many methods have been reported for measuring ET function. However, because no standard method is available, currently available tests have been regarded as incomplete and unreliable when used to make clinical decisions in patients with chronic otitis media (4, 15). In the present study, we found a positive relationship between preoperative ET functional measurements using a modified pressure equilibration method and postoperative middle ear aeration, although our technique did not comprehensively explore ET function.
In conclusion, ET function measured by a modified pressure equilibration test using an inflation-deflation manometric method was a good indicator of middle ear aeration and was predictive of better postoperative hearing.