CSF Otorrhea Resulting from Osteoradionecrosis of the Temporal Bone in a Patient with Recurrent Meningioma
Article information
Abstract
Osteoradionecrosis of the temporal bone is a very rare but potentially lethal complication of radiotherapy for head and neck or skull base tumors. Only two cases of osteoradionecrosis of the temporal bone complicating cerebrospinal fluid (CSF) otorrhea have been reported in the literature. This report describes a case of CSF otorrhea and osteoradionecrosis of the temporal bone in a patient with meningioma who was treated with tympanomastoid surgery and autologous fat obliteration in the mastoid.
INTRODUCTION
Osteoradionecrosis is a well-recognized complication of radiotherapy for head and neck or skull base tumors. It may predispose the patient to an aggressive or chronic infectious process and meningitis, or cause destruction of tissue by direct necrosis. The temporal bone is rare site of osteoradionecrosis; it is common in the mandible (1). Only two cases of osteoradionecrosis of the temporal bone complicating cerebrospinal fluid (CSF) otorrhea have been reported in the literature, and were in the cases with nasopharyngeal carcinoma (2, 3).
This case is the first report of CSF otorrhea from osteoradionecrosis of the temporal bone in a patient with recurrent meningioma. The patient was successfully treated with tympanomastoid surgery and autologous fat obliteration in the mastoid.
CASE REPORT
A 58-yr-old woman was diagnosed with meningioma at the right cerebello-pontine angle and underwent total tumor removal by a neurosurgeon in August 2002. Three years after the surgery, the tumor recurred and the patient received 5,400 cGy of radiation. Immediately after the completion of radiation therapy, otorrhea developed suddenly and had lasted for about 7 months when the patient was referred to the otolaryngology department in April 2006. Otoscopic examination of the right ear revealed clear pulsating discharge and a central perforation of the tympanic membrane.
Computed tomography (CT) of temporal bone demonstrated hyperostosis with sclerotic and lytic changes consistent with osteoradionecrosis. The inner margin of the cortical bone was destroyed and a moth-eaten appearance was identified at the superior margin of the petrous temporal bone (Fig. 1). The mastoid antrum and middle ear cavity were filled with soft tissue density. The T2 weighted magnetic resonance (MR) imaging showed high signal intensity, whereas T1 weighted MR imaging showed low signal intensity, suggesting CSF (Fig. 2). Despite 2 weeks of antibiotic medication and local treatment, the amount and nature of aural discharge did not change. Pseudomonas aeruginosa was isolated from the aural discharge. The aural discharge was collected and β2-transferrin under immunofixation electrophoresis was positive. Dry glucose test of the aural discharge was 52 mg/dL, implying again that it could be CSF. However, the radioisotope cisternography with Tc-99m did not reveal a specific leakage site.
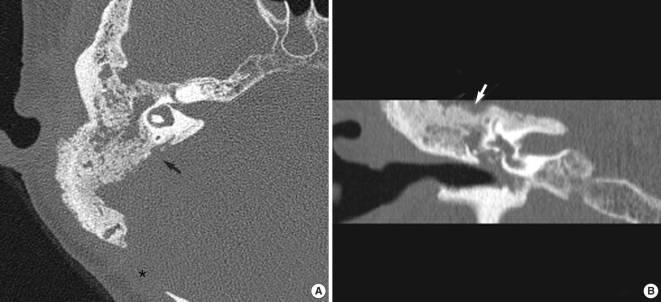
The axial (A) & coronal (B) temporal bone CT shows hyperostosis with sclerotic and lytic areas, and a moth-eaten appearance of the petrous portion of the right temporal bone, which was neighboring with the recurrent meningoma site (black and white arrow). The asterisk mark represents a defect from the previous operation.
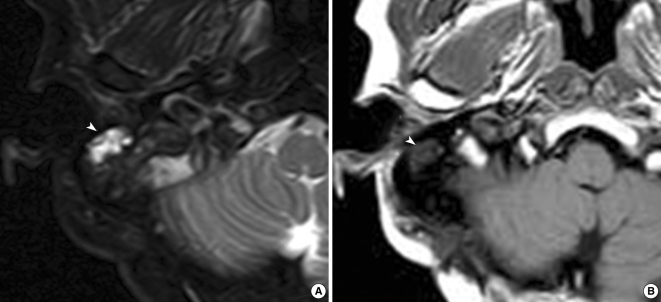
The T2 weighted MR image shows high signal intensity (A), whereas the T1 weighted MR image shows low signal intensity (arrowhead) (B).
A canal wall up mastoidectomy and exploration of the mastoid antrum was carried out in June 2006. The cortical bone of the mastoid process and mastoid tegmen was very soft and fragile. The mastoid cavity was filled with clear fluid. Although no definite tegmen defect was noted in the CT scans, there was an approximately 10 mm-sized, irregular margined shallow bony defect on the mastoid tegmen, and the exposed dura appeared relatively intact. No other defect or dehiscence was found under microscopic and rigid otoscopic examination. The defect on the tegmen and mastoid antrum was obliterated using autologous abdominal fat graft. The mucosa in the middle ear cavity was edematous. The ossiclular chain was intact. The tympanic membrane was reconstructed with type I tympanoplasty. Postoperativley, there has been no evidence of CSF leakage for 10 mon under otoscopic and nasopharyngeal examination.
DISCUSSION
The pathogenesis of osteoradionecrosis was first described by Ewing in 1926 (4). The first case of osteoradionecrosis of the temporal bone was reported by Block in a patient with syringobulba in 1952 (5). An aseptic, avascular necrosis of the bony tissue with obliterative vasculitis and arteritis is the main pathogenesis, and this is more likely to occur in the presence of tumor involvement. As osteolysis proceeds, demineralization of the bone with a compensatory reparative fibrosis occurs in the absence of osteoblastic activity. The tissue then becomes prone to injury and highly susceptible to infection. After infection sets in, the necrotic process accelerates and osteoradionecrosis continues. The severity of necrosis is closely correlated to the total amount of radiation. In this case, the recurrent tumor was closely approximated with temporal bone, possibly increasing the exposure to a relatively high dose of radiation. Osteoradionecrosis of the temporal bone was classified as either a localized or diffuse type by Ramsden et al. (1). In the localized type, osteoradionecrosis is generally confined to the external auditory canal, and symptoms usually include dermatitis, otalgia, and otorrhea. In the diffuse type, the disease extends beyond the temporal bone to the skull base. This type of disease can produce more severe symptoms including profuse and pulsatile otorrhea, and significant pain and can also be a more severe complication (2). Osteoradionecrosis of the temporal bone can make complications like hearing loss, gross tissue extrusion, chronic otomastoiditis, as well as more severe complications including meningitis, facial palsy, intradural and/or extradural abscesses, pneumocephalus, lateral sinus thrombosis, fistula formation into the parotid gland or temporal mandibular joint, and other cranial neuropathies (6). In this patient, the disease was relatively diffuse involving mostly the mastoid bone but not the deep skull base. The patient presented with an exceptionally rare complication of osteoradionecrosis of the temporal bone, secondary to radiotherapy for meningioma: an otogenic CSF leak. In this case, β2-transferrin was identified and a dry glucose test of the collected discharge suggested it could be CSF, although an isotope cisternogram study could not find the leakage site. This patient had a tympanic membrane perforation. However, considering the lack of otologic problems before radiotherapy, the perforation could have been caused by radionecrosis and/or subsequent infection. The patient was first treated conservatively with antibiotics and aural cleansing, but long-lasting clear aural fluid despite conservative treatment implied that it was a CSF leak. On the other hand, it is conceivable that recurrent meningioma may destroy the temporal bone resulting in CSF leakage. In this case, preoperative CT imaging study did not show a destructive pattern of the temporal bone but rather typical hyperostosis with sclerotic and lytic changes and small mastoid tegmen defect which was detected in operation might be caused by lytic change.
The management of osteoradionecrosis in the temporal bone is controversial. In the localized type, conservative treatment with frequent aural cleansing and topical antibiotics is often administered (7). In the presence of CSF leakage, conservative management such as bed rest, head elevation and, insertion of a subarachnoid drain can be useful. But for an unresponding case or the diffuse type, surgical management is indicated. Surgical management of osteoradionecrosis of the temporal bone has met with limited success because of the difficulty of accurate assessment of the viability of non-necrotic bone. Failure to resect all non-viable bone results in recurrence of a necrotic focus (8). In this case, we removed all inflamed, sponge-like non-viable bone that corresponded to the radionecrosis and closed the defect with autologous abdominal fat.