Treatment Efficacy of Various Maneuvers for Lateral Canal Benign Paroxysmal Positional Vertigo With Apogeotropic Nystagmus: A Randomized Controlled Trial
Article information
Abstract
Objectives.
The aim of this study was to determine the most effective treatment approach by comparing the impacts of various otolith reduction techniques in patients with apogeotropic lateral semicircular canal benign paroxysmal positional vertigo (LC-BPPV).
Methods.
We performed a multicenter randomized prospective study from January to December 2015, involving 72 consecutive patients with apogeotropic LC-BPPV. The patients were divided into three treatment groups: therapeutic head-shaking (group A), the Gufoni-Appiani maneuver (group B), and the cupulolith repositioning maneuver (CuRM; group C). Each group underwent evaluation and treatment up to the fourth week. Treatment success was defined as the disappearance of positional vertigo and nystagmus.
Results.
This study included 72 patients (49 male and 23 female), with a mean (±standard deviation) age of 55.4±13.5 years. The mean duration of vertigo experienced prior to treatment was 3.9±4.4 days. The mean latency and duration of nystagmus were 2.7±3.0 seconds and 47.9±15.8 seconds, respectively. The overall treatment frequency was 2.0±0.9. The number of treatments differed significantly among the three groups (P<0.05). After 4 weeks, the success rates for groups A, B, and C were 90.5%, 92.3%, and 100%, respectively. No significant difference was observed in the success rate across treatment methods and periods (P>0.05). However, CuRM was the only method with a 100% treatment success rate.
Conclusion.
While no clear difference was observed among the three treatments for LC-BPPV, CuRM was found to be superior to the other approaches in the long term.
INTRODUCTION
Benign paroxysmal positional vertigo (BPPV) is a condition in which a specific head position triggers stimulation of the semicircular canal. Due to the position of the otolith in the ampulla or semicircular canal, this stimulation results in severe vertigo and recognizable nystagmus [1]. Reports indicate that 18% of patients visiting dizziness clinics have BPPV. The lifetime prevalence of this condition is 2.4%, while the 1-year prevalence rate is 0.6% [2].
Based on the affected semicircular canal, BPPV can be categorized into posterior semicircular canal BPPV (PC-BPPV), lateral semicircular canal BPPV (LC-BPPV), and superior semicircular canal BPPV (SC-BPPV). The most common type is PC-BPPV, accounting for 80%–90% of cases, followed by LC-BPPV (10%–20%) and SC-BPPV (approximately 5%) [3]. LC-BPPV is characterized by severe rotational vertigo and nystagmus that occur when the head or body is turned while lying down; these symptoms result from the anatomical orientation of the LC [4].
LC-BPPV is diagnosed based on the characteristic nystagmus observed during the supine roll test (SRT). In this test, the patient’s head is turned to the left and right while in the supine position. The primary symptoms of BPPV that affect the LC are positional vertigo and direction-changing horizontal nystagmus [5]. The direction of the nystagmus during the SRT allows for the classification of LC-BPPV into two types: geotropic and apogeotropic nystagmus. The geotropic nystagmus type (LC-geo) accounts for most cases of LC-BPPV. It is associated with the presence of otoliths in the posterior arm of the LC and can be effectively treated with otolith reduction techniques such as the canalith repositioning maneuver or the Gufoni maneuver. In contrast, the apogeotropic nystagmus type (LC-apo) of LC-BPPV is believed to be caused by the presence of an otolith in the anterior arm of the LC or an otolith attached to the cupula (cupulolithiasis) [4]. Cupulolithiasis can be further categorized into two subtypes based on whether the otolith is attached to the utricular side or the canal side of the cupula. As such, a total of three subtypes of LC-apo exist [6-8].
The primary treatment strategy for BPPV involves moving the otolith into the utricle space. Since the location of the otolith differs across the three types of LC-apo, each necessitates a distinct method for transferring the otolith to the utricular space. (1) If the otolith is situated in the anterior arm of the semicircular canal, an initial maneuver is required to relocate the otolith to the posterior arm, thereby transforming it into the geotropic type. Following this, the condition can be treated with a maneuver designed for LC-geo. (2) In cases of cupulolithiasis on the canal side, a maneuver is initially required to dislodge the otolith from the cupula. Subsequently, it should be moved to the posterior arm for the application of LC-geo therapy. (3) In instances of cupulolithiasis on the utricular side, treatment can be administered by dislodging the otolith from the cupula and relocating it into the utricular space.
Theoretically, as previously mentioned, a treatment specific to each subtype should be selected. However, the challenge lies in the fact that no diagnostic test has been capable of pinpointing the precise location of otoliths within LC-apo. The efficacy of treatment for LC-apo is considerably lower than that for LC-geo. This discrepancy is primarily attributed to the use of non-specific treatment methods, which are utilized without knowledge of the exact location of the otolith.
To date, the reported treatment methods for apo-LC-BPPV can be categorized into two groups. First, based on the assumption of cupulolithiasis as the etiology, treatments including therapeutic head-shaking (THS) [9], the Gufoni-Appiani maneuver [10], forced prolonged position, and vibrator application have been suggested [11]. In 2005, Appiani modified the Gufoni maneuver to convert an apogeotropic to a geotropic LC-BPPV [10]. A recent study by an Italian group on the treatment of LC-BPPV indicated the Gufoni-Appiani maneuver as the most effective treatment for the apogeotropic type [12]. These maneuvers are primarily aimed to detach the otoliths from the cupula. The second group of treatments focuses on separating the otolith, enabling it to enter the semicircular canal, and returning it to the utricle. These techniques include the 360° canalith repositioning procedure (CRP) [13], the cupulolith repositioning maneuver (CuRM) [14], and the modified Semont maneuver [15].
In this study, we evaluated the treatment efficacy of three methods: (1) THS; (2) the Gufoni-Appiani method, which falls under the first category mentioned above; and (3) CuRM, which falls within the second category. Given that CuRM theoretically accomplishes both the dropping and repositioning of otolith particles in a single treatment session, it is reasonable to anticipate that the treatment efficacy of CuRM could surpass that of the other two maneuvers. The objective of this study was to determine the most effective treatment method by comparing the impacts of various otolith reduction techniques on patients with apogeotropic LC-BPPV.
MATERIALS AND METHODS
Patients
This study was a multicenter, prospective, randomized controlled study in which 17 researchers from 15 institutions from the Otological Research Interests Group in Korea participated. Between January and December 2015, 72 consecutive patients with apogeotropic LC-BPPV were recruited. The inclusion criteria were as follows: (1) history of vertigo associated with changes in head position, (2) horizontal apogeotropic nystagmus detected with Frenzel glasses or video goggles in SRT, (3) absence of spontaneous nystagmus, (4) vertigo associated with nystagmus, and (5) primary BPPV. The exclusion criteria were (1) neurologic diseases related to positional nystagmus or vertigo, (2) other accompanying inner ear disorders, (3) history of head trauma, (4) multicanal involvement, and (5) previous treatment with the CRP.
The study protocol was reviewed and approved by the Institutional Review Boards of each institution of participants and followed the tenets of the Declaration of Helsinki. Informed consent was obtained from all the patients (Catholic Medical Center, No. XC13EIMI0119O).
Study design
This was a prospective, randomized trial consisting of three treatment groups. Patients who met the inclusion criteria were included in the study, and primary treatment was performed according to a random assignment table. We divided the treatment groups into three groups: THS (group A), the Gufoni-Appiani maneuver for apogeotropic nystagmus (group B), and the CuRM (group C). Three patients in each group recovered during the course of treatment. There were no subjects with follow-up loss (Fig. 1). After each treatment, no specific postural restriction existed, and antihistamines, tranquilizers, and antiemetic drugs were not prescribed (Fig. 2). We recorded the symptoms, the direction of nystagmus (geotropic/apogeotropic), latency, and duration of nystagmus for up to 60 seconds at each treatment. The total CRP number and treatment duration for successful treatment were also evaluated.

Flow diagram illustrating the effects of various otolith reduction techniques in patients with apogeotropic lateral semicircular canal benign paroxysmal positional vertigo. THS, therapeutic head-shaking; CuRM, cupulolith repositioning maneuver.
Evaluation and successful treatment results
The SRT was performed 20 minutes after treatment. If the nystagmus and rotational vertigo disappear, it is considered a “treatment success.” If the apogeotropic nystagmus persisted, the assigned treatment maneuver for each group was performed again, and the patient was followed up one week later. In the case of nystagmus conversion to the geotropic direction, the Barbecue maneuver for geotropic LC-BPPV was performed to group A and C. The Gufoni maneuver for geotropic LC-BPPV was performed to group B. After the second treatment, weekly assessment and treatment were performed until last assessment at 4th week. Treatment was repeated until positional vertigo and nystagmus was not evoked by SRT. If apogeotropic nystagmus was still induced by SRT at 4 weeks, it was determined as treatment failure.
Diagnostic procedure
The clinician selects cases in which rotational vertigo is induced by head movement, and induced vertigo disappears within 1–2 min. Spontaneous nystagmus, Dix-Hallpike test, and SRT were performed while wearing Frenzel glasses to diagnose BPPV and identify the affected semicircular canals. The diagnostic procedure was performed prior to each treatment session as follows.
Spontaneous nystagmus was first observed. The patient was brought from a sitting to a supine position, and the presence or absence of lying-down nystagmus (LDN) was observed. If specific nystagmus is present, the direction of nystagmus is checked until it disappears. When the nystagmus disappeared, the patient’s head was turned 90° to the right, and vertigo symptoms and nystagmus were checked. The clinician recorded the latency, duration, and geotropic/apogeotropic direction of nystagmus. When nystagmus disappeared, the head returned to its center. If the nystagmus does not disappear after a while, it waits up to 1 min and then turns to the center. If nystagmus disappeared with the head in the central position, the head was turned 90° to the left and examined in the same manner.
The lesion side was diagnosed as follows: when apogeotropic nystagmus was present on SRT, the direction of nystagmus with LDN was considered to be the affected lesion, and when there was no LDN, the direction of weak nystagmus was considered to be the affected lesion [16]. If geotropic nystagmus appeared in the SRT, the opposite direction of the nystagmus in the LDN was on the affected side. If there was no LDN, the side with the strongest nystagmus was determined to be the affected side.
Treatment procedure
Therapeutic head-shaking
To keep the LC parallel to the plane of rotation, the patients lay down with their heads bent at 30° [9,17]. The clinician held the patient’s head and shook it at an angle of 30° to the left and right at a rate of 2 Hz for 15 seconds. Following the procedure, the patient lay down for 2 minutes.
Gufoni-Appiani maneuver
The patient is seated in the center of the treatment table. Next, the patient quickly lays on the side with the affected ear down. Maintain this position until the nystagmus disappears. Turn the patient’s head 45° upward quickly and hold in this position for 2 minutes. Slowly return to a sitting position [10,12,18].
Cupulolith repositioning maneuver
In the supine position, the head was quickly turned 90° toward the affected side. Place a vibrator (60 Hz) on the posterosuperior part of the affected ear for 30 seconds and maintain this position for 2 minutes. Quickly turn the head 90° toward the normal side (upright position) and hold for 2 minutes. The head was quickly turned 90° toward the normal side (position of the affected ear facing the ceiling), a vibrator (60 Hz) was placed on the posterosuperior part of the affected ear for 30 seconds, and this position was maintained for 2 minutes. Quickly turn the head 90° toward the normal side (prone) and hold this position for 2 minutes. Sit slowly with the patient’s head slightly bowed [19,20].
Statistical analysis
Chi-square and Kruskal-Wallis tests were used to compare the clinical characteristics of the patients allocated to each treatment group and to determine the therapeutic efficacy of the three groups. All statistical analyses were performed using SPSS ver. 12.0 (SPSS Inc.), and statistical significance was set at P<0.05.
RESULTS
Patient characteristics
This study included a total of 72 patients (49 male and 23 female), with a mean (±standard deviation [SD]) age of 55.4±13.5 years. The mean duration of vertigo experienced by these patients prior to treatment was 3.9±4.4 days. The right side was more commonly affected, with a prevalence ratio of 1.8:1. The latency of nystagmus was recorded at 2.7±3.0 seconds, while its duration was measured at 47.9±15.8 seconds.
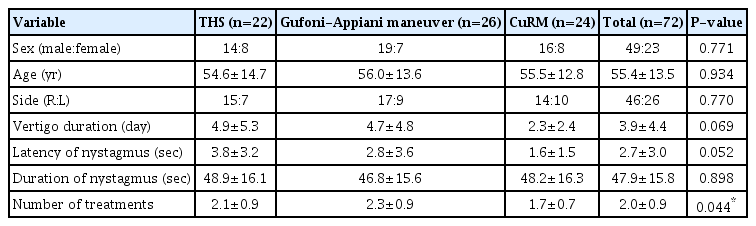
The study groups A, B, and C comprised 22, 26, and 24 patients, respectively. No significant differences were observed in sex, age, affected side, duration of vertigo latency of nystagmus, or duration of nystagmus among these groups. The mean (±SD) number of repositioning maneuvers required for successful treatment was 2.0±0.9. Group C (mean±SD, 1.7±0.7), required significantly fewer treatments than groups A (mean±SD, 2.1± 0.9) and B (mean±SD, 2.3±0.9) (P<0.05) (Table 1).
Treatment success rate
The cumulative success rate did not significantly vary among the three groups for any assessment period. The overall success rate was 94.4% after 4 weeks. By treatment group, the success rates at the final assessment in week 4 were 90.5% (group A), 92.3% (group B), and 100% (group C). No significant difference in the success rate was observed among the treatment methods and periods (P>0.05). However, CuRM was the only method with a 100% treatment success rate (Table 2, Fig. 3). All patients in group C were successfully treated within 2 weeks, demonstrating rapid and superior treatment efficacy. In the head-shaking and Gufoni-Appiani groups, approximately 10% of patients continued to exhibit apogeotropic nystagmus or vertigo and were classified as cases of treatment failure.
DISCUSSION
The most notable finding of this study was that the total number of treatments required to reduce otoliths and achieve successful treatment was significantly lower in group C than in the other groups (P<0.05). Group C demonstrated a 100% cure rate at the 2-week mark, and this success was achieved more rapidly than with other treatment methods. Consequently, CuRM is indicated to be the most effective method for treating apogeotropic LC-BPPV.
Despite the proposal of various diagnostic methods and treatment modalities, it remains challenging to confirm the type of apogeotropic LC-BPPV. Additionally, not all types have standardized treatments. The treatment success rate for LC-BPPV following various repositioning maneuvers is relatively low (70%–80%) due to discrepancies among the subtypes [14,21]. In fact, when the Korean Otology Society surveyed the treatment modalities for apogeotropic LC-BPPV, they found approximately 20 different methods in use. This revealed a striking diversity in treatment combinations compared to those used for posterior canal BPPV and geotropic LC-BPPV [20].
While the exact prevalence of each subtype of LC-BPPV remains undetermined, it is generally believed that the utricular form is particularly common. Shim et al. proposed that in the natural progression of LC-BPPV, patients with the apo-type experienced a notably quicker relief of symptoms compared to those with the geo-type. This quicker alleviation of symptoms in apo-LC-BPPV compared to geo-LC-BPPV implies that the utricular type of cupulolithiasis (CUP-U) may be the primary cause of apo LC-BPPV, rather than the canal type of cupulolithiasis (CUP-C) or canalithiasis in the anterior arm of the lateral canal (CAN) [22].
Ramos et al. identified three subtypes of the apogeotropic type of LC-BPPV, based on the nystagmus observed during the first and second steps of Zuma’s treatment maneuver [23]. If the particles are in the CAN, a transient nystagmus with a contralesional direction will be observed at both steps. If the particles fall under the CUP-C subtype, a prolonged nystagmus with a contralesional direction will be observed at both steps. For the CUP-U subtype, persistent nystagmus will be observed at both steps, with the direction of the nystagmus changing from contralesional at step 1 to ipsilesional at step 2. In that study of 18 patients, the CAN subtype was found in eight patients, the CUP-C subtype in six patients, and the CUP-U subtype in three patients. The pathway to the utricle is notably short in the CUP-U subtype, which may lead to spontaneous symptom remission. The researchers proposed that this was the reason why utricular side cupulolithiasis was observed in relatively few patients in their study [8].
The 360° CRP [13], Kim’s maneuver [14], and Zuma’s maneuver [23] can be used to treat all three types of conditions using a single method. However, the specific type is not known in advance, necessitating the observation of nystagmus direction in both the supine and opposite side-lying positions throughout the treatment process. The Gufoni-Appiani method can be utilized for treating CUP-C or CAN, while the modified Semont maneuver is beneficial for treating CUP-U [15]. The Gufoni-Appiani method, the forced prolonged position, and the THS maneuver are deliberating maneuvers. Although the maneuver is what causes the otolith to drop, it can also be viewed as a therapeutic maneuver since it allows the otolith to enter the utricle when returning to a sitting position.
A recent study evaluated the therapeutic efficacy of CuRM in treating apogeotropic LC-BPPV, comparing it with the THS and modified Lempert maneuvers. This double-blinded randomized prospective study revealed no significant differences in clinical characteristics across the three groups. Furthermore, the therapeutic effects observed on the second day and 1-week posttreatment were consistent across all groups [17]. These findings align with the results of our study, which also indicated no significant differences among the three groups. However, discrepancies were observed between the previous study and ours in terms of the observation period and recovery rate. In our study, group C demonstrated a 100% treatment success rate after 2 weeks, suggesting that treatment with a vibrator may be the most effective approach. After 4 weeks of treatment, all treatments resulted in a recovery rate exceeding 90%, a figure that may be influenced by the course of natural recovery. In a separate study, Kim et al. [14] assessed 78 patients with persistent apogeotropic LC-BPPV and administered CuRM. They reported a treatment success rate of 97.4%, with a mean of 2.1 repetitions, a finding that is consistent with our results. The authors proposed that CuRM is an effective treatment method for apogeotropic LC-BPPV [14].
Limited reports are available on the success rate of THS. Oh et al. [9] conducted a prospective randomized trial to evaluate the therapeutic efficacy of the relevant maneuvers in apogeotropic LC-BPPV. They compared the immediate efficacies of the THS and modified Semont maneuvers in a sample of 103 consecutive patients with apogeotropic LC-BPPV. Their findings indicated that THS was more effective than the modified Semont maneuver (37.3% vs. 17.3%, P=0.02). The superior effectiveness of THS as the initial treatment for apogeotropic LC-BPPV, regardless of the side of attachment, may be attributed to its capacity to alternately accelerate and decelerate, thereby separating the otoliths from the cupula [9]. Kong et al. [17] reported a resolution rate of 12.5% following a single application of the THS technique on the first day. However, the success rate rose to 75% after 1 week. In our study, the initial success rate of THS was 18.2%, and it increased to 71.4% after 1 week. However, the treatment failure rate of THS was 10.5% in group A in week 4, which is a lower failure rate than reported in other studies. These discrepancies may be due to differences in treatment periods.
Several studies have been conducted on the Gufoni-Appiani maneuver. Ciniglio Appiani et al. [10] assessed the effectiveness of the maneuver in treating apogeotropic LC-BPPV. All patients underwent a repositioning procedure, which was based on the presence of free-floating dense particles in the endolymph of the anterior arm of the lateral canal. The LC-BPPV in all patients transitioned from an apogeotropic to a geotropic variant following the repositioning procedure. This process facilitates the movement of the otolith from the anterior to the posterior arm of the lateral canal [10]. Kim et al. [24] performed a randomized prospective sham-controlled study to assess the therapeutic efficacy of the Gufoni-Appiani and head-shaking maneuvers in treating apogeotropic LC-BPPV. Patients were randomly assigned to the Gufoni-Appiani (n=52), head-shaking (n=54), or sham maneuver (n=51) groups and were followed up weekly for 1 month after the initial maneuver. Relative to the sham maneuver, both the Gufoni-Appiani (P<0.001) and head-shaking maneuvers (P=0.026) demonstrated superior cumulative therapeutic benefits. However, no significant difference was reported in the short-term (P=0.128) or long-term (P=0.239) results between the Gufoni-Appiani and head-shaking groups in terms of therapeutic efficacy [24].
The effectiveness of oscillations during repositioning maneuvers remains a topic of discussion. Mastoid oscillations are applied to the affected ear during the particle repositioning maneuver, with the aim of returning the otoliths to the utricle by preventing their adherence to the cupula or canal [25,26]. While performing this repositioning maneuver, Li [25] underscored the importance of oscillations. In that prospective study, Li [25] found that 70% of patients in the vibration group experienced a resolution of nystagmus, compared to none in the vibration-free group. Conversely, Oh et al. [9] performed mastoid oscillation in conjunction with the Brandt-Daroff exercise and found no additional benefit for patients with apogeotropic LC-BPPV. Other prior studies have also indicated no significant effect of mastoid oscillation [26,27]. Moreover, CuRM exhibited the highest treatment success rate of 38.9% after its initial application on the first day. The resolution rate of CuRM demonstrated a significant improvement on the second day. This treatment success is believed to be due to the effective repositioning of both otoliths in the anterior arms of the LC and the detachment of the otoliths from the cupula through oscillation.
The present study had several limitations. First, the sample size for each cohort was relatively small. Future research with a larger participant pool is therefore required. Second, the previous literature has indicated a male-to-female sex ratio of 1:2 or 1:3, depending on the clinical characteristics of BPPV. However, this study observed a reversal in the gender ratio, with a male predominance of 2.1:1. LC-BPPV accounts for approximately 10% of all BPPV cases, and among them, apogeotropic LC-BPPV is relatively infrequently encountered. This could explain the observed reversal in the male-to-female ratio. Third, the study sample may have been subject to selection bias. Category 1 therapy (THS and the Gufoni-Appiani maneuver) merely dislodges the otolith from the cupula, rather than completely removing it from the canal, which could result in a comparatively weak therapeutic efficacy. Category 2 therapy (CuRM) involves both dislodging the otolith and repositioning it, potentially leading to a higher treatment efficacy than the other two maneuvers. Fourth, it is challenging to differentiate between the subtypes of LC-BPPV at the time of diagnosis. While the subtype can be predicted during treatment, further research into subtype diagnosis would be beneficial for the treatment of patients with apo-LC-BPPV.
We performed a multicenter randomized controlled study to validate the efficacy of oscillations in treating persistent apogeotropic LC-BPPV. As such, we compared the therapeutic efficacy of CuRM with other therapeutic maneuvers. We conclude that oscillation, as demonstrated by the CuRM results, effectively dislodged otoliths from the cupula. Despite the lack of observed difference between the groups in terms of recovery rate after a 1-month follow-up period, group C exhibited the fastest and highest recovery rates, as well as the fewest treatments. While no clear difference was observed between the three treatments for LC-BPPV, CuRM demonstrates relative superiority over the other treatment methods in long-term effectiveness.
HIGHLIGHTS
▪ The apogeotropic form of lateral semicircular canal benign paroxysmal positional vertigo (LC-BPPV) can be attributed to the presence of free-floating particles in the anterior arm of the LC, particles adhering to the cupula within the canal, or particles attached to the cupula within the utricle.
▪ No significant difference exists in the treatment success rate among the three methods used to treat apogeotropic LC-BPPV.
▪ Over the long term, the cupulolith repositioning maneuver demonstrates superiority compared to other treatments.
Notes
No potential conflict of interest relevant to this article was reported.
AUTHOR CONTRIBUTIONS
Conceptualization: JEJ, JWH. Data curation: JEJ, NS, MSK, YSY, BSH, CJW, CJH, HSM, LSH, KMB, KJW, KHJ, SJH, ASK, PSN, KM, CWH. Formal analysis: JEJ, LHJ. Methodology: JEJ, LHJ. Project administration: JEJ, NS, CWH. Visualization: JEJ, LHJ. Writing–original draft: JEJ, LHJ. Writing–review & editing: JEJ, LHJ.
Acknowledgements
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korean government (MIST) (No. RS-2023-00210073).
Statistical consultation was supported by the Department of Biostatistics of the Catholic Research Coordinating Center.