|
 |
- Search
AbstractObjectivesSince few studies on surgical training and learning curves have been performed, majority of inexperienced surgeons are anxious about performing operations. We aimed to access the results and learning curve of septoplasty with radiofrequency volume reduction (RFVR) of the inferior turbinate.
MethodsWe included 270 patients who underwent septoplasty with RFVR of the inferior turbinate by 6 inexperienced surgeons between January 2009 and July 2011. We analyzed success score, cases of revision, cases of complication, operation time, and acoustic rhinometry.
ResultsSuccess score was relatively high and every surgeon had few cases of revision and complication. No significant difference was found in success score, revision, complication case, or acoustic rhinometry values between early cases and later cases. Operation time decreased according to increase in experience. However, there was no significant difference in the operation time after more than 30 cases.
Septoplasty is one of the most commonly performed rhinologic procedure and basic surgery that should be learned. However, the learning of septoplasty is quite difficult due to limited surgical view, diverse deviations of nasal septum and few hands-on practice courses. Therefore, septoplasty is hard to be trained, and inexperienced surgeons have a fear of unsatisfactory results and side effects such as a saddle nose and septal perforation.
The studies of learning curve have been mostly done about laparoscopic surgery and financial aspects for training residents in Western countries [1-4]. In the field of rhinology, the study of learning curve was usually performed about endoscopic sinus surgery [5-7]. To date, only two studies about learning curve of septoplasty were addressed [8,9]. One study focused on introducing the quick septoplasty technique and compared the results of only two surgeons; a senior and junior surgeon [9]. The other study didn't include enough cases to compare the results and the authors classified groups into surgeon's level, even though the cases of each surgeon's level were different [8]. Furthermore, all of two articles didn't deal with the satisfaction of patients and the degree of correction which are most important result of the surgery.
Since deviation of nasal septum mostly accompanies hypertrophy of inferior turbinate, septoplasty is usually performed with turbinoplasty. However, no study about learning curve of septoplasty with turbinoplasty exists.
Therefore, we wished to know the surgical results and learning curves of septoplasty with turbinoplasty performed by several inexperienced surgeons.
Between January 2009 and July 2011, patients who underwent septoplasty with turbinoplasty (due to deviation of nasal septum with inferior turbinate hypertrophy and a complaint of nasal obstruction) in our department were included in this study. Exclusion criteria included a follow-up period of less than a year and inadequate chart records. During the period, 6 surgeons, who were ENT residents trained in our department, began to perform septoplasty with turbinoplasty during the second year of their practice and continued the surgery until their fourth year. Three surgeons (surgeons A, B, and C) operated on between 30 and 60 patients, while the other 3 surgeons (surgeons D, E, and F) conducted operations on over 60 patients. We included the first 30 patients of surgeons A, B, and C and the first 60 patients of surgeons D, E, and F, using the sequential order of the operations performed. Therefore, a total of 270 patients and 6 inexperienced surgeons were included in this study. The patients recruited to this study were combined and stratified into several groups to allow comparison of surgical results.
Success score, cases of revision, cases of complication, operation time, and acoustic rhinometry values were analyzed by a retrospective chart review. Success score was rated on a 3-point numerical scale according to assessment by a senior surgeon (JSK), and the degree of symptom improvement as rated by the patients (3, well corrected deviation of the nasal septum and no nasal obstruction; 2, existence of remnant deviation or partially relieved nasal obstruction; 1, poorly corrected deviation and no symptom improvement). If patients complained of persistence of nasal obstruction and prominent septal deviation was observed in spite of surgery, revision septoplasty was conducted by the senior surgeon. All revision operations were performed within a year from the first operation, which is within a follow-up period of this study. Surgical complications included septal perforation, hematoma, septal abscess, synechia, saddle nose, and postoperative bleeding. Operation time was recorded in minutes and defined as the period from draping of the patient to packing of the nasal cavity. Minimal cross-sectional area (MCA) gap and volume gap were used to analyze the outcome of acoustic rhinometry. MCA gap is defined as the difference between the preoperative MCA value of acoustic rhinometry on the convex side of the septum and the postoperative MCA value. Volume gap is defined as the difference between the preoperative volume value (up to 5.4 cm) of acoustic rhinometry on the convex side of the septum and the postoperative volume value.
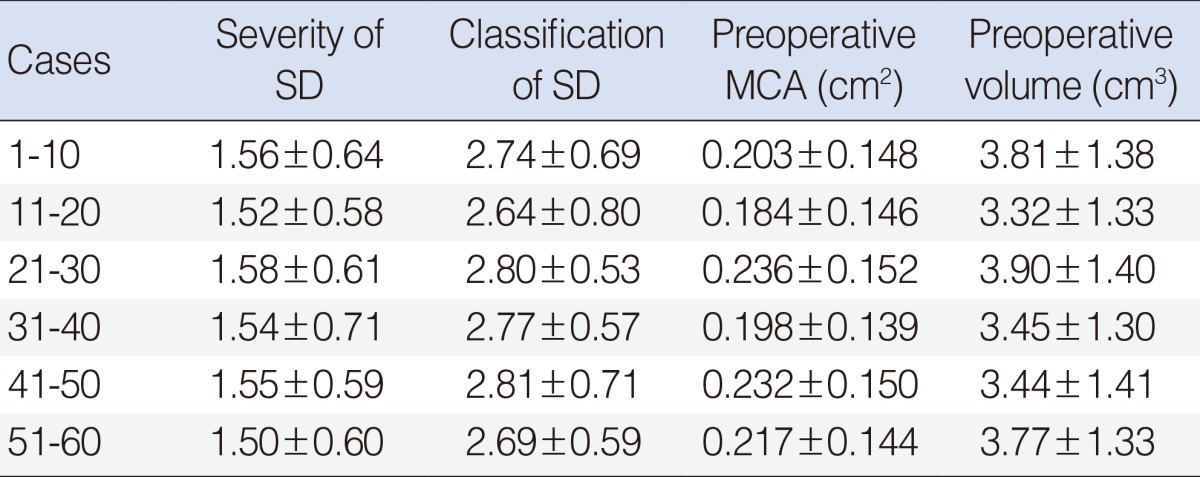
Since all patients were assigned to the surgeons in sequential order of operation, a selection bias did not occur. In order to confirm an absence of the bias, severity and classification of septal deviation as well as the value of preoperative acoustic rhinometry were compared between the groups. Severity of septal deviation were classified into 3 types and rated on 3-point numerical scale for the comparison (Table 1). Classification of septal deviation was stratified into 4 types and rated on 4-point numerical scale (Table 2). These classification systems for septal deviation (Tables 1, 2) were proposed by Jin et al. [10]. and we modified it by rating the types on a numerical scale.
Septoplasty was performed under local anesthesia, except in the first patient of each surgeon. During the first surgery of each training surgeon, the senior surgeon guided and taught techniques to the training surgeon under general anesthesia. After local infiltration, hemitransfixion incision was performed on the concave side of the nasal septum. The mucoperichondrium and mucoperiosteum flaps were elevated, and separation between the cartilaginous and bony portions of the septum was carried out. Correction of the bony portion by fracturing and removing the overlapping portion was performed and the crest or spur as well as any excessive septal cartilage were trimmed. Then, the septum was repositioned into the midline and an anchoring suture was carried out to fix the septum into central portion. Lastly, the flap was closed with sutures, and quilting sutures and nasal packing were performed to prevent hematoma.
Septoplasty was followed by turbinoplasty. The turbinoplasty technique involved radiofrequency volume reduction (RFVR) with a coblator (ReFlex 45 wand, Arthrocare Co., Sunnyvale, CA, USA). Coblation was performed at several sites for 4 to 10 seconds depending on the degree of hypertrophy of the inferior turbinate, with the power output level set to 4.
Data were analyzed using SPSS ver. 18.0 (SPSS Inc., Chicago, IL, USA). Success score were tested using Mann-Whitney test. Operation time and acoustic rhinometry values (MCA, and volume) were tested with unpaired t-test. Cases of revision and complication were tested with Fisher exact test. Kruskal-Wallis test (for scores of severity and classification of septal deviation) and one-way analysis of variance (ANOVA; for preoperative acoustic rhinometry values) were used to analyze the differences between early cases and later cases in order to avoid the possible bias that early patients may have been easier cases. Differences were considered significant when the P-value was <0.05.
In baseline characteristics of total 270 patients, the number of male and female was 173 and 97, respectively. A mean age was 35.7±14.0 years (range, 15 to 78 years) and a mean period of postoperative follow-up was 23.1±7.1 months (range, 12 to 42 months).
No significant improvements in success score, cases of revision, cases of complication, or acoustic rhinometry values were shown between the first, second, and third 10 cases of the combined cases of surgeons A, B, C, D, E, and F (Table 3). Cases of complication during second 10 cases (2 cases of 60) were fewer than that of during first 10 cases (7 cases of 60), but there was no statistical difference (P=0.163). Among the 7 cases of complication occurred during first 10 cases, synechia, septal perforation, and epistaxis happened in 4, 2, and 1 case, respectively. Since the size of synechia and septal perforation was small, the patients did not present symptoms including nasal obstruction, crust, whistling sound. Therefore, operation for correcting a complication was not performed. Operation time decreased consecutively in accordance with an increase in operated cases and it was statistically significant (between first and second 10 cases, P=0.013; between second and third 10 cases, P=0.003).
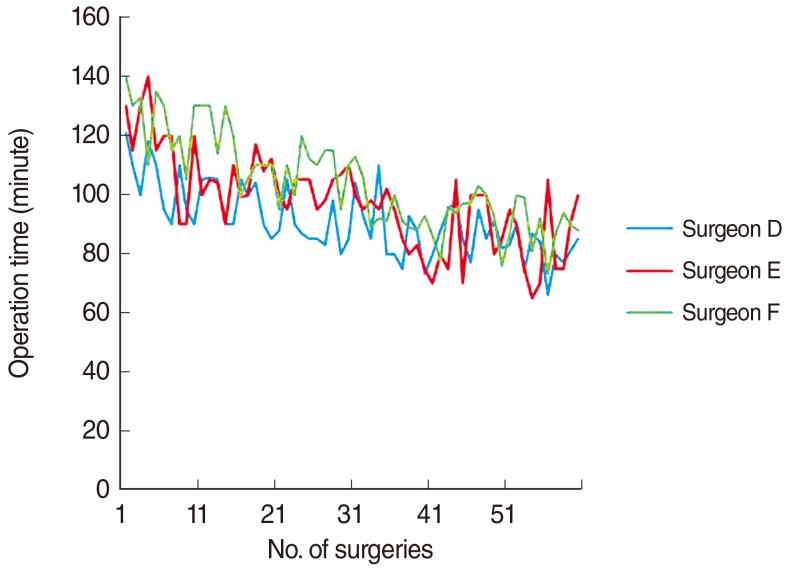
The combined cases of surgeons D, E, and F were analyzed in order to determine learning curve (Table 4). The analysis showed that only operation time was consistently decreased with experience. A statistically significant decrease in operation time was showed up to 30 cases. After 30 cases, the operation time continued to decrease, but no statistical significance was shown. Fig. 1 also shows that decline in operation time was steep up to 30 cases, but then became more gradual over the next 30 cases. Comparison of each 10 cases indicated that success score, cases of revision, cases of complication, MCA gap, and volume gape were not significantly improved. However, the incidence of complication was meaningfully decreased between the first 10 cases (6 cases of 30) and the groups with more than 30 cases (no case of 30; P=0.024).
Kruskal-Wallis test and ANOVA revealed that there were no significant differences in the score of the degree of septal deviation and preoperative MCA and volume acoustic rhinometry values between early cases and later cases (from first to sixth 10 cases) of the 6 surgeons (Table 5).
Deviation of the nasal septum is a common anatomic variation and frequently causes nasal obstruction. Septoplasty is needed to relieve the uncomfortable symptom of nasal obstruction. Although septoplasty is a basic surgery, learning to perform this procedure is very difficult for the following reasons. First, the surgical view of septoplasty is highly limited. Although endoscopic septoplasty has recently been performed by some surgeons, the majority of septoplasty is conducted with the naked eye. Therefore, even the main assistants of this surgery cannot sufficiently observe the procedure due to a limited view. Second, deviation of the septum differs between individuals and various types of deviation exist. For this reason, diverse techniques are required as the occasion demands [11,12]. Third, unlike endoscopic sinus surgery and rhinoplasty, few hands-on practice courses for septoplasty are held. Hands-on practice courses teach basic surgical anatomy and techniques as well as the experiences of senior surgeons. However, the availability of septoplasty practice courses is not abundant compared to other surgeries.
In addition to the reasons mentioned above, insufficient studies on the learning curve and operation results of inexperienced surgeons cause anxiety about performing septoplasty in unskilled and beginner surgeons. The first study on the learning curve of septoplasty was performed by Liu et al. [8] in 2009. They included 4 ENT surgeons trained in the same tertiary referral medical center from the second to fifth year of their practice. The patients of the 4 surgeons were combined and assessed regarding average operation time, hospital stay, and complications. Three minor complications occurred and these were handled easily. Therefore, the authors concluded that septoplasty is an easy and safe procedure. However, they came to the conclusion that it takes 5 years to train a surgeon to perform septoplasty without giving a proper reason or explanation. Furthermore, since the patient numbers of each level of surgeon ranged from 12 to 23, comparison of the results by surgeon level may have led to inaccurate analyses. To avoid these possible drawbacks, we stratified our patients into groups according to the order that operation was performed, since operation order reflects the experience of the surgeon. The second study by D'Ascanio and Manzini [9] analyzed the operation time of septoplasty according to sequence of operation, but the authors included only 1 senior and 1 junior surgeon, and did not compare other surgical results such as the degree of correction of the nasal septum, symptom improvement, and acoustic rhinometry values. In addition, they focused on introducing a septoplasty technique called quick septoplasty.
In this study, we included 6 surgeons and analyzed their surgical results according to the order of the surgeries performed. As we expected, wih accumulation of surgical experience, the operation time of all of the surgeons decreased continuously. However, unexpectedly success score, cases of revision, cases of complication, and acoustic rhinometry values were not significantly different between patients operated on at an early stage and those operated on later. Even the results of the first 10 cases were satisfactory and comparable with the cases performed later. The occurrence of few cases of revision (6 out of 270 cases operated on by inexperienced surgeons) indicates that septoplasty with RFVR of the inferior turbinate performed by unskilled operators results in satisfactory surgical outcomes. Consequently, we concluded that septoplasty is a safe surgery with satisfactory results even when performed by inexperienced surgeons.
In order to assess the learning curve of septoplasty, we combined the cases of surgeons D, E, and F and stratified them into 6 groups of 10 cases, from the first to the sixth 10 cases. Operation time significantly decreased up to 30 cases, but there was no statistical difference between the third and the fourth 10 cases, the fourth and the fifth 10 cases, or the fifth and the sixth 10 cases. The graph showing the operation time of the 3 surgeons (Fig. 1) indicates that the operation time reached a plateau after 30 operations. There were also statistically more complications in the first 10 cases than in the groups with more than 30 cases. Therefore, we can assume that 30 cases are needed in order for a surgeon to become relatively skillful at septoplasty with RFVR.
Since this is the first study to report the number of cases involved in the learning curve of septoplasty, we cannot compare our results with previous investigations. In studies on other surgeries, Smith et al. [13] reported that the surgical results of endoscopic transsphenoidal skull base surgery reached a plateau between 18 and 34 cases. According to Soot et al. [14], 25 cases were required to attain surgical proficiency of laparoscopic fundoplication. For aural atresia surgery, a learning curve of 32 ears was required to achieve stable short-term hearing results [15]. A learning curve of sialendoscopy was also achieved at 30 cases [16]. Although different surgeries show different learning curves, our results had a similar learning curve to several other surgeries.
There are some possible limitations to interpreting the results of this study. First, since the range of success score, from 1 to 3, was narrow, it is possible that success score did not sufficiently reflect the success of the surgery. Therefore, we are now prospectively studying the learning curve of septoplasty with RFVR of the inferior turbinate by including visual analogue scale scores, from 1 to 10, for symptom improvement and a greater number of surgeons. Second, the accuracy and ability of acoustic rhinometry to determine the degree of nasal obstruction are controversial [17,18]. However, acoustic rhinometry is still a useful tool to objectively detect the degree of septal deviation, and is widely used for treatment as well as investigational studies. Third, there is a possibility that the surgeons selected easier cases when they were in a more inexperienced state. Moreover, the severity and classification of septal deviation could affect the result of operation time. Therefore, we analyzed the differences in the score of the degree of septal deviation and preoperative acoustic rhinometry values between the early and later 10 cases (from first to sixth 10 cases) of the 6 surgeons with Kruskal-Wallis test and ANOVA. No difference existed between the groups. Therefore, easier cases were not assigned to more inexperienced surgeons. In reality, the patients were randomly allocated to the surgeons regardless of the level of difficulty.
There are many kinds of technique for septoplasty with turbinoplasty. Even in the same type of surgery, different techniques can have various learning curves. Moreover, the training centers of institutions have different curriculums for training inexperienced surgeons. Trainees are exposed to different training methods according to their circumstances. Therefore, we hope more studies on learning curves involving various types of surgery technique and training institutions will be carried out in the future in order to provide more information on the learning curve of septoplasty with turbinoplasty.
Very satisfactory surgical results for septoplasty with RFVR performed by inexperienced surgeons were shown in this study. There were few cases of revision and complication, and success score was higher than we expected. Furthermore, operation time decreased consistently according to accumulation of surgical experience. Surgical outcomes reached a plateau over 30 cases. We can conclude that surgeons who start to learn septoplasty with RFVR do not need to fear of failure and complications, and merely need more time to operate when compared with experienced surgeons.
ACKNOWLEDGMENTSWe would like to acknowledge the support of Biostatistics Unit, Kyungpook National University (Assistant professor, Won Kee Lee, PhD) for statistical analyses and interpretation of data.
References1. Babineau TJ, Becker J, Gibbons G, Sentovich S, Hess D, Robertson S, et al. The "cost" of operative training for surgical residents. Arch Surg. 2004 4;139(4):366-369. PMID: 15078701.
2. Bridges M, Diamond DL. The financial impact of teaching surgical residents in the operating room. Am J Surg. 1999 1;177(1):28-32. PMID: 10037304.
3. Koperna T. How long do we need teaching in the operating room? The true costs of achieving surgical routine. Langenbecks Arch Surg. 2004 6;389(3):204-208. PMID: 14557883.
4. Wang MC, Yu EC, Shiao AS, Liao WH, Liu CY. The costs and quality of operative training for residents in tympanoplasty type I. Acta Otolaryngol. 2009 5;129(5):512-514. PMID: 18720069.
5. Bokhari AR, Davies MA, Diamond T. Endoscopic transsphenoidal pituitary surgery: a single surgeon experience and the learning curve. Br J Neurosurg. 2013 2;27(1):44-49. PMID: 22900510.
6. Marks SC. Learning curve in endoscopic sinus surgery. Otolaryngol Head Neck Surg. 1999 2;120(2):215-218. PMID: 9949355.
7. Uribe JI, Ralph WM Jr, Glaser AY, Fried MP. Learning curves, acquisition, and retention of skills trained with the endoscopic sinus surgery simulator. Am J Rhinol. 2004;Mar-Apr;18(2):87-92. PMID: 15152873.
8. Liu CY, Yu EC, Lin SH, Wang YP, Wang MC. Learning curve of septomeatoplasty. Auris Nasus Larynx. 2009 12;36(6):661-664. PMID: 19414230.
9. D'Ascanio L, Manzini M. Quick septoplasty: surgical technique and learning curve. Aesthetic Plast Surg. 2009 11;33(6):814-818. PMID: 19582504.
10. Jin HR, Lee JY, Jung WJ. New description method and classification system for septal deviation. J Rhinol. 2007 5;14(1):27-31.
11. Dobratz EJ, Park SS. Septoplasty pearls. Otolaryngol Clin North Am. 2009 6;42(3):527-537. PMID: 19486747.
12. Fettman N, Sanford T, Sindwani R. Surgical management of the deviated septum: techniques in septoplasty. Otolaryngol Clin North Am. 2009 4;42(2):241-252. PMID: 19328889.
13. Smith SJ, Eralil G, Woon K, Sama A, Dow G, Robertson I. Light at the end of the tunnel: the learning curve associated with endoscopic transsphenoidal skull base surgery. Skull Base. 2010 3;20(2):69-74. PMID: 20808530.
14. Soot SJ, Eshraghi N, Farahmand M, Sheppard BC, Deveney CW. Transition from open to laparoscopic fundoplication: the learning curve. Arch Surg. 1999 3;134(3):278-281. PMID: 10088568.
15. Patel N, Shelton C. The surgical learning curve in aural atresia surgery. Laryngoscope. 2007 1;117(1):67-73. PMID: 17202933.
16. Luers JC, Damm M, Klussmann JP, Beutner D. The learning curve of sialendoscopy with modular sialendoscopes: a single surgeon's experience. Arch Otolaryngol Head Neck Surg. 2010 8;136(8):762-765. PMID: 20566901.
17. Cakmak O, Tarhan E, Coskun M, Cankurtaran M, Celik H. Acoustic rhinometry: accuracy and ability to detect changes in passage area at different locations in the nasal cavity. Ann Otol Rhinol Laryngol. 2005 12;114(12):949-957. PMID: 16425563.
18. Roithmann R, Cole P, Chapnik J, Barreto SM, Szalai JP, Zamel N. Acoustic rhinometry, rhinomanometry, and the sensation of nasal patency: a correlative study. J Otolaryngol. 1994 12;23(6):454-458. PMID: 7897780.
Table 1Types of severity for septal deviation 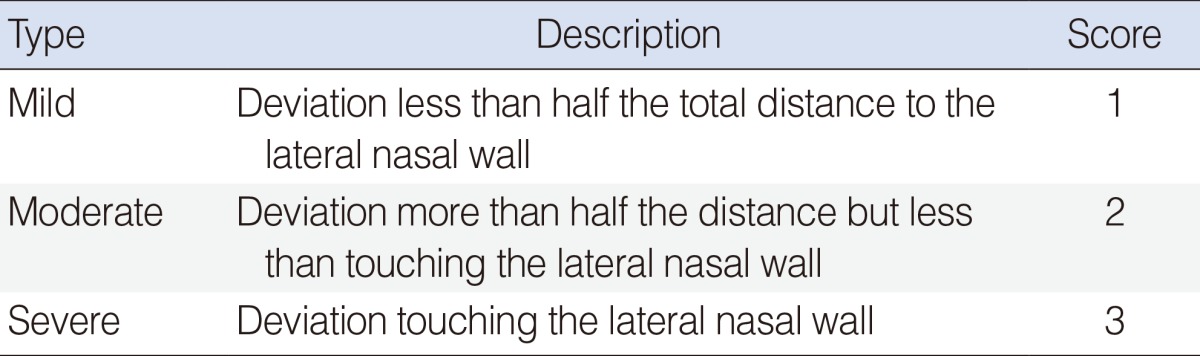 The types of severity for septal deviation were proposed by Jin et al. [10] and we modified it by rating the types on a numerical scale. Table 2Types of classification of septal deviation  The types of classification of septal deviation were proposed by Jin et al. [10] and we modified it by rating the types on a numerical scale. Table 3Surgical outcomes and statistical analysis of septoplasty with RFVR of the inferior turbinate for combined cases (surgeons A-F) 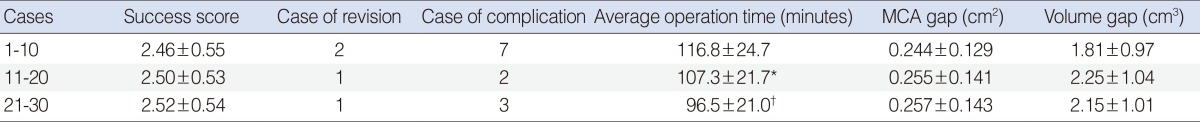
Table 4Surgical outcomes and statistical analysis of septoplasty with RFVR of the inferior turbinate for combined cases (surgeons D-F) to assess the learning curve 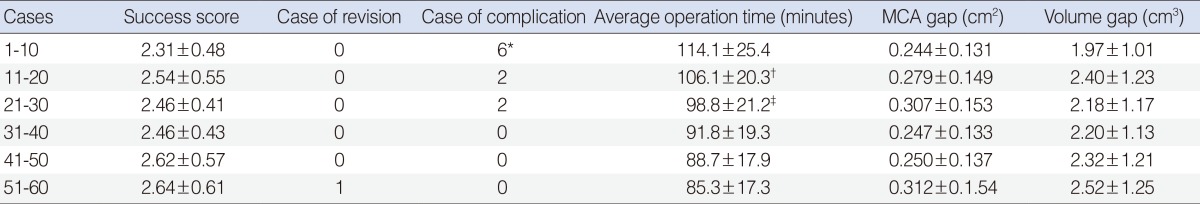 RFVR, radiofrequency volume reduction; MCA, minimal cross-sectional area. *P=0.024 vs. the groups of more than 30 cases (cases of 31-40, 41-50, and 51-60); †P=0.049 vs. the group of cases of 1-10; ‡P=0.038 vs. the group of cases of 11-20; Other values showed no significant differences compared to those of following 10 cases. |
|
||||||||||||||||||||||||||||||||||||||