Comparison between Real-Time Ultrasound-guided Percutaneous Dilatational Tracheostomy and Surgical Tracheostomy in critically ill Patients: A Randomized Controlled Trial
Article information
Abstract
Objectives.
Tracheostomy is an important procedure for critically ill patients in the intensive care unit (ICU), and percutaneous dilatational tracheostomy (PDT) has gained popularity due to its safety and effectiveness. However, there are limited data comparing ultrasound-guided PDT (US-PDT) with surgical tracheostomy (ST). In our previous study, we reported that US-PDT had similar safety and effectiveness to ST, with a shorter procedure time. However, the study design was retrospective, and the sample size was small. Therefore, we conducted a randomized controlled trial to demonstrate the safety and efficacy of US-PDT compared to ST.
Methods.
A total of 70 patients who underwent either US-PDT (n=35) or ST (n=35) were enrolled in the study between October 20, 2020 and July 26, 2022. The patients were randomly assigned to their respective procedures. The data collected included patient clinical characteristics, procedure time and details, complications, duration of ICU stay, time taken for weaning from mechanical ventilation, and hospital mortality.
Results.
The procedure time of US-PDT was shorter than that of ST (4.0±2.2 minutes vs. 10.1±4.6 minutes). The incision length of US-PDT was also shorter than that of ST (1.5±0.5 cm vs. 1.8±0.4 cm). There were no statistically significant differences in demographics, procedure details, complications, length of ICU stay, ventilator weaning time, and hospital mortality.
Conclusion.
US-PDT has a similar complication rate and shorter procedure time compared with ST. It can be safely and effectively performed in critically ill patients and can serve as a potential alternative to ST.
INTRODUCTION
Tracheostomy is an important procedure in critically ill intensive care unit (ICU) patients, and its incidence is increasing due to the growing demand for mechanical ventilation in ICU patients [1]. Open surgical tracheostomy (ST) is the standard procedure, offering optimal lighting and exposure of the surgical field [2]. However, ST is associated with a relatively high incidence of surgical site infections, unfavorable scarring, and perioperative bleeding [3,4]. Percutaneous dilatational tracheostomy (PDT), which was first described by Ciaglia et al. in 1985 [5], is now widely used due to its expected safety and efficacy. Several studies have shown that PDT is not inferior to ST in terms of complications and has the advantages of being an easy and fast procedure, labor- and cost-efficient, and safe because there is no need to transport patients to the operating room [6,7].
Bronchoscopy-guided PDT is widely used because it can identify the location of the trachea during puncture and prevent damage to the posterior tracheal wall [8]. However, it can be challenging to identify cervical anatomical structures, such as vessels or the thyroid, and it requires a bronchoscope to be used by a specialist [9,10]. In contrast, ultrasound-guided PDT (US-PDT) is expected to have advantages, including portability and safety, due to its ability to identify anatomical structures [11]. Several studies have demonstrated the advantages of real-time ultrasound compared to bronchoscopy [9-13]. However, there are limited data available comparing US-PDT with ST.
In our last retrospective study, we reported that US-PDT had similar safety and effectiveness to ST, with a shorter procedure time [14]. However, due to the retrospective design and small sample size of that study, we conducted a randomized controlled trial to further demonstrate the safety and efficacy of US-PDT compared to ST.
MATERIALS AND METHODS
Trial design
This prospective, randomized controlled trial was conducted at a single center (Soonchunhyang University) between October 20, 2020 and July 26, 2022. Study procedures were followed in accordance with the Helsinki Declaration of 1975. The study protocol was approved by the Institutional Review Board of Soonchunhyang University, Bucheon (Approved on October 14, 2020, No. SCHBC 2020-05-028) and registered with the Korean Clinical Research Information Service (Registered on June 27, 2023, registration number KCT0008564). Written informed consent was obtained from all patients or their legal representatives if the patient was not mentally alert. All procedures were performed by a single head and neck surgeon with over 15 years of experience in tracheostomy. The sample size was estimated based on previous studies (14.4 minutes in ST group and 10.2 minutes in US-PDT group) [12,13]. With a study power of 0.8 and an alpha error of 0.05, 34 patients per group were required for the sample size. Assuming a low dropout rate, 70 patients were enrolled and randomly allocated into either the US-PDT (n=35) or the ST (n=35) group using a computer-generated randomized sequence. Two patients were excluded post-procedure due to consent withdrawal, resulting in a final inclusion of 68 patients.
Patients
Adult patients who required prolonged intubation, pulmonary toilet, airway protection due to neurologic disease or traumatic brain injury, or adjunct tracheostomy to major head and neck surgery or airway obstruction were eligible to participate. Exclusion criteria included age younger than 19 years, a history of cervical surgery, tracheostomy, or irradiation, emergent tracheostomy, severe coagulopathy or hemodynamic instability with anticoagulant or antiplatelet drugs that cannot be stopped for at least 2 days, anterior cervical mass, infection at the puncture site, and COVID-19 infection. Severe coagulopathy or hemodynamic instability was defined as an overall score of more than 2 points, with 1 point each for a platelet count <100,000/mm3, prothrombin time increase >3 seconds, activated partial prothrombin time increase >5 seconds, fibrinogen <150 mg/dL, fibrin degradation product increase, and D-dimer increase.
Ultrasound-guided PDT
The Ciaglia Blue Rhino tracheostomy kit (Cook Medical Inc.) was used for the US-PDT procedure. After marking the anatomical landmarks through palpation and injecting local anesthesia (2% lidocaine containing 1:100,000 epinephrine), real-time ultrasound was used to identify the optimal level of tracheal puncture. The medical staff then deflated the balloon of the endotracheal tube (E-tube) and slowly withdrew it to just above the level of puncture under ultrasound guidance. During the repositioning of the E-tube, the tip of the E-tube was identified through combined approaches, including double linear hyperechogenicity of the E-tube, saline ballooning after deflation of air, and anterior protrusion of the tracheal wall by the E-tube tip (Fig. 1A and B) [14]. After repositioning the E-tube, a guide needle was inserted with ultrasound guidance to identify the midline and avoid injury to vascular structures. Confirmation of whether the guide needle was positioned in the tracheal lumen was done by regurgitation of air into a saline-filled syringe (Fig. 1C and D). A guide wire was then introduced through the needle, and a horizontal skin incision was made after the removal of the needle. A dilator was inserted over the guide wire, and after multiple dilations, an appropriately sized tracheostomy tube (T-tube) (7 mm for women, 8 mm for men) was inserted. Confirmation of the endotracheal placement of the T-tube was done by portable fiberoptic laryngoscope. The procedure details are illustrated in our previous study [14]. The entire procedure was performed by a single head and neck surgeon with only one medical staff member for E-tube repositioning. The first T-tube change was performed after 1 week and was regularly changed every 2 weeks.
(A, B) Following the real-time ultrasound-guided repositioning of the endotracheal tube, the tip of the E-tube is observed to push the tracheal wall anteriorly at the level of the second tracheal ring. (C, D) A guide needle is inserted into the midline of the trachea under ultrasound guidance. Correct needle positioning within the tracheal lumen is confirmed by observing the regurgitation of air into a saline-filled syringe. C, cricoid cartilage; T2, second tracheal ring.
Surgical tracheostomy
The ST was performed using a conventional procedure. After injecting local anesthesia (2% lidocaine containing 1:100,000 epinephrine), a horizontal skin incision was made, and sharp and blunt dissection was used to expose the trachea. The isthmus of the thyroid was partially divided to achieve optimal exposure for creating a tracheal window. The window was made between the second and third tracheal ring, and a T-tube was inserted. Confirmation of endotracheal placement of the T-tube was done by using a portable fiberoptic laryngoscope. The T-tube was changed in the same way as with US-PDT.
Data collection
The following data were collected in this study: age, sex, weight, height, body mass index (BMI), Acute Physiology and Chronic Health Evaluation (APACHE) II score, inner diameter of the E-tube, indication for tracheostomy, anatomical difficulties, duration of intubation, presence of tracheal deviation, and limited neck extension. The procedure-related data collected were as follows: the distance from the lower border of the cricoid cartilage to the sternal notch, the distance from the skin to the second tracheal ring, and the tracheal diameter measured by ultrasound; the depth of the E-tube from the mouth before the procedure in both groups, and the depth of the repositioned E-tube in the US-PDT group; the length of the skin incision; the number of guide needle and puncture site corrections in the US-PDT group; the estimated blood loss; the ease of the procedure (rated as easy, somewhat difficult, difficult, very difficult, or impossible); the preparation time (defined as the time from betadine sterilization to the complete preparation of all equipment); the procedure time; and the inner diameter of the T-tube.
The following data were collected after the procedure: information regarding complications, duration of stay in the ICU, time required to wean from mechanical ventilation, and number and cause of hospital mortality. The procedure time was defined as the time elapsed from E-tube repositioning to T-tube insertion in the US-PDT group, and from skin incision to T-tube insertion in the ST group. In the US-PDT group, the duration for E-tube repositioning was also measured and recorded as USG duration.
Complications were classified as major or minor. Major complications were defined as: hypotension (systolic blood pressure below 90 mmHg for more than 5 minutes or any interventions required to increase blood pressure), acute hypoxemia (peripheral oxygen saturation below 90% for more than 5 minutes), major bleeding (requiring transfusion or surgical intervention), pneumothorax, injury to the tracheal wall or esophagus, loss of airway, accidental decannulation, false passage cannulation, cardiac arrest, and death associated with the tracheostomy procedure. Minor complications were defined as: transient hypotension (systolic blood pressure below 90 mmHg for less than 5 minutes), transient hypoxemia (peripheral oxygen saturation below 90% for less than 5 minutes), minor bleeding (localized and easily controlled by local compression or topical vasoconstrictive drugs), localized emphysema, atelectasis, and inadvertent cuff puncture. Complications were monitored for at least 3 months after the procedure.
Statistical analysis
IBM SPSS 26.0 (IBM Corp.) was used for statistical analysis of the collected data. The normality of numeric parameters was assessed using normality tests, and then compared using the Student t-test. Non-numeric parameters were analyzed using the chi-square test. Statistical significance was assumed at a P-value of less than 0.05.
RESULTS
Between October 20, 2020 and July 26, 2022, 100 patients were screened for eligibility. Of these, 30 were excluded, and 70 were randomized. The most common indication for tracheostomy was the need for prolonged ventilation, followed by pulmonary toilet. Two patients were excluded after the procedure because they withdrew their consent. Ultimately, 68 patients were included, with 35 in the ST group and 33 in the US-PDT group (Fig. 2).
Flowchart of patient enrollment. ST, surgical tracheostomy; US-PDT, ultrasound-guided percutaneous dilatational tracheostomy.
Patients who dropped out were managed as follows: Those with a history of tracheostomy or cervical surgery received ST. Patients with severe coagulopathy underwent US-PDT if platelet count was <50,000/mm3. For patients with platelet counts between 50,000/mm3 and 100,000/mm3, the choice between ST and US-PDT was based on the surgeon’s discretion. Patients with a history of irradiation also received tracheostomy according to the surgeon’s preference.
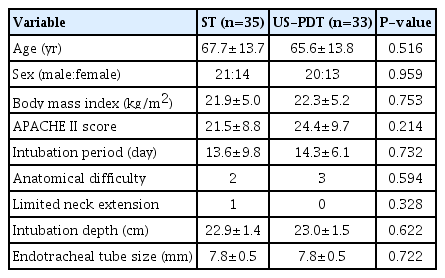
Table 1 presents the data collected before the procedure. There were no significant differences in age, sex, BMI, APACHE II score, and duration of intubation between the groups. Anatomical difficulties were present in two patients in the ST group and three patients in the US-PDT group. Limited neck extension was found in one patient in the ST group. The depth of intubation and size of the endotracheal tube were not significantly different between the two groups.
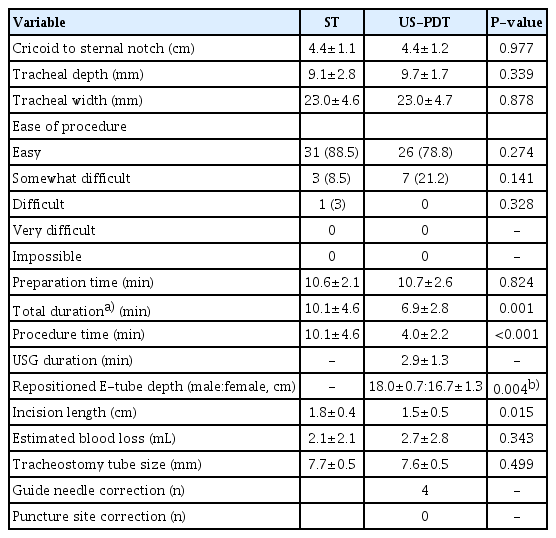
Table 2 presents procedure-related data. There were no significant differences between groups in terms of cricoid-sternal notch distance, tracheal depth, and tracheal width. In the ST group, 88.5% of the procedures were rated as easy, 8.5% were somewhat difficult, and 3% were difficult. ST was difficult in one patient due to severe tracheal cartilage ossification, and somewhat difficult in three patients who were obese and had short neck. In the US-PDT group, 78.8% of the procedures were rated as easy and 21.2% were somewhat difficult, with most of the somewhat difficult cases due to challenging dilation caused by tracheal ossification. There was no significant difference in preparation time between the two groups. The procedure time of the US-PDT group was 4.0±2.2 minutes, which was significantly shorter than that of 10.1±4.6 minutes in the US-PDT group (P<0.001). The total duration, including the procedure time and the time for USG-guided E-tube repositioning, was 6.9±2.8 minutes in the US-PDT group, which was also significantly shorter than that of the ST group (P=0.001). The repositioned E-tube depth was 18.0± 0.7 cm in men and 16.7±1.3 cm in women in the US-PDT group (P=0.004). The incision length in the ST group was 1.8±0.4 cm, while it was 1.5±0.5 cm in the US-PDT group, which was statistically significant (P=0.015). There were no differences between the groups in estimated blood loss and size of the T-tube. In the US-PDT group, the guide wire was kinked during dilation in four patients, but easily reinserted. There was no need for puncture site correction in the US-PDT group.
Table 3 presents the complications and data collected after the procedure. There were no major complications in either group, and the complication rate did not differ significantly between the groups. False lumen insertion occurred in only one patient in the US-PDT group, but reinsertion was successful without life-threatening complications. Transient desaturation occurred in eight patients (three in the ST group and five in the US-PDT group), and local subcutaneous emphysema occurred in three patients (one in the ST group and two in the US-PDT group). Bleeding occurred in one patient each in both groups, and it was easily controlled by local gauze compression with a topical vasoconstrictive drug. Infection was found in five patients (two in the ST group and three in the US-PDT group), and all cases were local stomal infections without sepsis. The time spent for weaning from mechanical ventilation and the length of ICU stay did not differ between the groups. Hospital mortality was also similar between the groups, and there were no tracheostomy-related deaths.
DISCUSSION
Since its description by Sustic in 1999 [15], the use of US-PDT has been increasingly adopted and many studies have demonstrated its efficacy and safety [16-19]. One of the advantages of real-time ultrasonography is the ability to identify vascular structures, the midline path of the needle, and the appropriate level of tracheal cartilage [19]. Sustic et al. [20] reported a lower incidence of cranial misplacement of the T-tube (placement between the cricoid cartilage and first tracheal ring) in the US-PDT group compared to blind PDT, and real-time ultrasonography can be useful in avoiding tracheal stenosis.
In this study, no case of US-PDT failure or conversion to ST was observed. Although Petiot et al. [21] reported a long learning curve associated with US-PDT, our study found that the ease of the procedure was similar between the two groups. Other studies also reported that US-PDT was considered easy or somewhat difficult in more than 87% of cases and is even included in resident training curricula [9,11]. Nonetheless, it is important to remain vigilant for the possibility of procedure failure and to be prepared for conversion to ST if necessary.
The procedure time for US-PDT was significantly shorter than that for ST (4.0±2.2 minutes vs. 10.1±4.6 minutes), even when considering the time required for USG-guided E-tube repositioning. Our findings are consistent with those of previous studies that reported US-PDT to be faster than ST [17,22]. The incision length for US-PDT was also shorter than that for ST (1.5±0.5 cm vs. 1.8±0.4 cm), indicating that US-PDT may have an advantage over ST in terms of avoiding unfavorable scarring, as reported in other meta-analyses [3].
The incidence of complications was similar between the two groups, and no major complications were observed. Similarly, mortality rates did not differ significantly between the groups. According to Cramer et al. [23], the tracheostomy-associated mortality rate in adult patients is 0.0022%. Although no tracheostomy-related deaths occurred in our study, this may be due to the small sample size. Other studies have reported that ST has a relatively higher risk of infection and bleeding [3,4]. However, in our study, the incidence of bleeding and infection was not significantly different between the two groups. This may be due to the meticulous bleeding control performed by the head and neck surgeon (with over 15 years of experience), regular and thorough stoma site dressing in the ICU, and the exclusion of patients with a high risk of bleeding or infection.
One case of false lumen insertion occurred during T-tube insertion in the US-PDT group, which was confirmed by a portable fiberoptic laryngoscope. However, since the puncture site was already established and the level was appropriate, the guide wire was reinserted, and the T-tube was successfully repositioned without any other complications.
In our study, we followed our institutional policy of performing the first T-tube change after 1 week, which is longer than the usual time frame of 3–7 days after tracheostomy [24]. This policy was implemented after accidents occurred with early first Ttube changes performed before 3 days after tracheostomy. Since the change in policy, there have been no accidents. Additionally, we did not include patients who underwent emergent tracheostomy in our study. However, a study by Ravi et al. [25] included 16 emergent cases of US-PDT and reported no failure, conversion to ST, major complications, or death, indicating that US-PDT can be safely used in emergency situations.
US-PDT offers several advantages over ST. Firstly, the procedure can be conducted under indirect vision, which can help to reduce aerosol generation and prevent viral transmission, such as COVID-19 [26]. Secondly, unlike ST, no surgical assistant is required, making US-PDT more efficient and potentially reducing the risk of infection due to fewer people being involved. Thirdly, US-PDT can be performed at the patient’s bedside in the ICU, eliminating the need to transport the patient to the operating room. This can be particularly beneficial for patients who are too ill to be moved safely.
Despite the limitations in sample size and short-term follow-up for complications, it is important to note that this is the first randomized controlled trial comparing ST and US-PDT. Further larger, multicenter studies are necessary to evaluate the long-term safety and efficacy of US-PDT.
The results of our study indicate that US-PDT has a similar complication rate and shorter procedure time compared with ST. Our findings suggest that US-PDT can be safely and effectively performed in critically ill patients and may be a potential alternative to ST.
HIGHLIGHTS
▪ Percutaneous dilatational tracheostomy (PDT) is widely used due to safety and efficacy.
▪ Ultrasound-guided PDT (US-PDT) has a shorter procedure time and incision length compared to surgical tracheostomy.
▪ US-PDT is a safe and effective option for tracheostomy in critically ill patients.
Notes
No potential conflict of interest relevant to this article was reported.
AUTHOR CONTRIBUTIONS
Conceptualization: KNP. Data curation: SYK, AB. Methodology: SWL, KNP. Writing–original draft: SYK, AB. Writing–review & editing: SWL, KNP.
Acknowledgements
This research was supported by the Soonchunhyang University Research Fund, the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (Grant no. 2017R1C1B5018147).